Preoperative and Postoperative N-terminal Pro B-type Natriuretic Peptide Levels Predict Cardiac Morbidity and Mortality in Patients Undergoing Colorectal Cancer Resection
Abstract
Introduction:
Cardiac complications are a major cause of perioperative morbidity and mortality in patients undergoing colorectal cancer surgery. A quick and reliable system for predicting postoperative cardiac morbidity is needed to predict cardiac events in order to improve outcome in surgery. The aim of this study was to investigate the role of the biochemical marker NT-proBNP in the prediction of postoperative all-cause mortality, cardiac-related mortality and cardiovascular events in patients undergoing colorectal cancer resections.
Methods:
100 consecutive patients undergoing colorectal cancer surgery were prospectively recruited. Blood samples were taken preoperatively, 24h, 48h and 5-7 postoperative days to measure NT-proBNP levels. The predictive power of NT-proBNP levels was assessed using Receiver Operating Characteristics (ROC) curves.
Results:
Cardiac-related morbidity and mortality was 9%. Of eleven deaths, 5 were cardiac-related. Preoperative NT-proBNP was a good predictor of death with ROC area under curve (AUC) of 0.83 (95% C.I. 0.673, 0.993) a strong predictor of cardiac death with AUC of 0.914 (95% C.I. 0.823, 1.000) and a good predictor of cardiac complications with AUC of 0.875 (95% C.I. 0.757, 0.993). NT-proBNP levels 24 hours and 48 hours postoperatively were also strongly predictive of postoperative cardiac morbidity and mortality.
Conclusion:
Pre- and postoperative NT-proBNP have a role in predicting postoperative death and cardiac complications. This may have significant implications in the planning of postoperative care for high-risk patients.
Author Contributions
Academic Editor: Leonardo Bustamante-Lopez, Sao Paulo University, Brazil
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2018 Haney Youssef, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Cardiac complications are a major cause of perioperative morbidity and mortality in patients undergoing colorectal cancer surgery.1The prediction of these cardiac events is notoriously difficult, but essential, as determining the stage of heart disease may lead to different management choices, such as angiotensin converting enzyme inhibitors or b blockers2. These treatments can delay or reverse progression of disease and therefore may improve prognosis by reducing postoperative complications.
One important aim of preoperative evaluation is to identify patients with significant coronary artery disease who may be at risk of cardiac complications following surgery. Many studies have looked into factors that might adversely affect these cardiac events and they include increasing age, New York Heart Association class, left ventricular ejection fractions, diabetes mellitus and lower blood pressure.3 Some of these risk indices have been developed into preoperative cardiac risk scoring systems such as revised cardiac risk index (RCRI)4 and Goldman cardiac index.5 Other methods of assessing cardiac risks such as dobutamine cardiac stress testing and echocardiography are highly sensitive but are expensive and often limited by time and availability of resources. Furthermore, the Government has set a challenging target for the NHS, that by December 2008, no patient should wait more than 18 weeks from the time of GP referral to the start of hospital treatment. These tests could potentially delay surgery and would therefore not be suitable for pre-operative surgical patients. A quick and reliable system for predicting postoperative cardiac morbidity is needed to predict cardiac events in order to improve the outcome of surgery.
Recent published literature has indicated that Brain Natriuretic Peptide (BNP) and its related compound, N-terminal fragment pro B-type Natriuretic Peptide (NT-proBNP), can be used to identify patients at high risk of developing major adverse cardiac events following non-cardiac surgery.6 BNP is synthesized by human cardiac myocytes as a 108-amino acid prohormone (proBNP), which is cleaved to the 32-residue BNP and the 76-residue NT-proBNP.7 Both BNP and NT-proBNP can be used as sensitive biomarkers of cardiac dysfunction7 and have been used as preoperative predictors of cardiac morbidity in cardiac8 and non-cardiac surgery6, 9, 10. The biochemical markers BNP and NT-proBNP are available as commercial assays.
The aim of this study was to investigate the role of the biochemical marker NT-proBNP in the prediction of postoperative all-cause mortality, cardiac-related mortality and cardiovascular events in patients undergoing colorectal cancer resections.
Methods
The study was approved by the regional ethics committee and hospital research and development department. Between September 2006 and October 2007, 100 consecutive patients undergoing elective colorectal cancer resection who gave consent were recruited to the study. All patients had preoperative cardiac risk stratification using the revised cardiac risk index, which stratifies patients into classes I – IV.4, Table 1 shows the risk index variables and the risk of cardiac complications for respective classes. Serum measurements were taken preoperatively and postoperatively at days 1, 2 and 5-7, for NT-proBNP and cardiac troponin-T (Tn-T). Clinical assessment and ECGs were also performed preoperatively and postoperatively at days 1, 2 and 5-7. To avoid bias, all tests and clinical assessments were performed by a clinical researcher who was not involved in patients’ care.
Table 1. Cardiac risk in Non-cardiac surgery according to the revised cardiac risk index4| Revised Cardiac Risk Index (RCRI) Class | Number of variables | Risk of Cardiac Complications (%) |
| I | 0 | 0.4 |
| II | 1 | 0.9 |
| III | 2 | 6.6 |
| IV | >2 | 11 |
| RCRI Variables: high-risk type of surgery, history of ischemic heart disease, history of congestive heart failure, history of cerebrovascular disease, preoperative treatment with insulin, and preoperative serum creatinine >2.0 mg/dL | ||
Cardiac complications included acute myocardial infarction, silent myocardial infarction, acute coronary syndrome, heart failure and cardiac arrhythmias. The diagnosis of heart failure required a clinical diagnosis of heart failure and radiological evidence of pulmonary oedema. All ECGs were read by an experienced consultant cardiologist. Where cardiac complications were identified by the researcher, this was communicated to the clinical team looking after the patient for immediate referral to a cardiologist.
Data were also prospectively collected on type of resection undertaken, postoperative histology and postoperative complications. Surgery was carried out by one of four colorectal firms in all cases.
Assay
Serum NT-proBNP levels were measured using a sandwich immunoassay principle utilising a biotinylated antibody; streptavidin-coated and streptavidin-coated microparticles, with electrochemical detection of the bound complex via the rare earth ruthenium. The normal NT-proBNP value using this assay is <40 pmol/L.
Statistics
The value of preoperative NT-proBNP, 24 hours postoperative NT-proBNP and 48 hours postoperative NT-proBNP levels as predictors for overall death, cardiac death and cardiac complications were assessed using Receiver Operator Characteristic (ROC) curves. The area under each ROC curve (i.e. AUC) was calculated. A perfect predictive score will be equal to one. A score showing good predictive value will have a value > 0.8. The sensitivities, specificities, negative predictive values (npv) and positive predictive values (ppv) were also calculated for NT-proBNP value cut-off levels of 40 pmol/L and 90 pmol/L.
Results
Of the 100 patients recruited, 66 were male and 34 were female, with a median age of 72 years (range 39-90). Table 2 shows the different types of colorectal operations performed along with their postoperative histology results.
Table 2. Baseline Patient characteristics| Characteristic | Number of Patients | |
| Operation | Right sided resection | 42 |
| Anterior resection | 36 | |
| APR | 5 | |
| Left sided other | 15 | |
| Other | 2 | |
| Postoperative histology | A | 13 |
| B | 51 | |
| C1 | 23 | |
| C2 | 10 | |
| Other | 3 | |
Adverse Outcomes
Of the 100 patients, there were 11 postoperative deaths, of which 5 were due to cardiac causes. These included 4 myocardial infarctions and one patient with acute left ventricular failure and atrial fibrillation. There were 9 patients with cardiac complications including the 5 cardiac-related deaths.
Table 3 shows the distribution of cardiac complications, cardiac deaths and other deaths according to risk stratification using the RCRI. Out of 76 patients stratified to RCRI class II, there were 2 cardiac deaths, 3 non-cardiac deaths and 4 cardiac complications (survivors). In this class of risk, this corresponded to a 7.9% (6/76) cardiac complication rate, compared with 0.9% predicted by the RCRI.
Table 3. The distribution of cardiac complications, cardiac deaths and other deaths according to risk stratification using the Revised Cardiac Risk Index (RCRI)| RCRI Class | Number of Patients | Cardiac complications-survivors | Cardiac deaths | Other deaths |
| I | 0 | 0 | 0 | 0 |
| II | 76 | 4 | 2 | 3 |
| III | 15 | 0 | 1 | 2 |
| IV | 9 | 0 | 2 | 1 |
The causes of non-cardiac death (n=6) were pneumonia (n=2), MRSA sepsis from necrotic toe (n=1), Clostridium difficile sepsis (n=1), diarrhoea sepsis (n=1) and sepsis leading to MOF (n=1).
Postoperative Tn-T
Tn-T levels were elevated in 11 patients within 1 week postoperatively. Death from MI accounted for 4, there were 2 silent MI’s, 4 mild Tn elevations indicating minor myocardial injury (but not diagnostic of myocardial infarction) and 1 mild elevation from a patient who died from pneumonia leading to multiorgan failure.
Preoperative NT-proBNP as a Predictor
For all-cause mortality, the ROC curve AUC was 0.83 (95% c.i. 0.673, 0.993), making preoperative NT-proBNP a good predictor of postoperative death (Figure 1).For cardiac death, the AUC was 0.914 (95% c.i. 0.823, 1.000), making preoperative NT-proBNP a very strong predictor of postoperative cardiac death (Figure 2).For cardiac complications (deaths and survivors) the AUC was 0.875 (95% c.i. 0.757, 0.993), making preoperative NT-proBNP a good predictor of postoperative cardiac complications (Figure 3).
Figure 1.Pre-operative NT-proBNP as a predictor of death
Figure 2.Pre-operative NT-proBNP as a predictor of cardiac death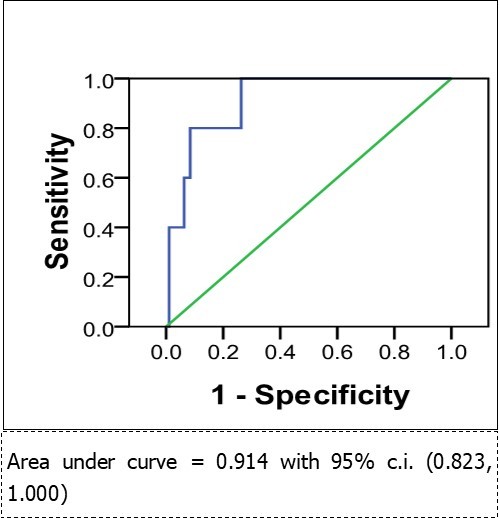
Figure 3.Pre-operative NT-proBNP as a predictor of cardiac complications
Postoperative NT-proBNP as a Predictor
NT-proBNP values 24h post op were poorly predictive of death from all causes with AUC=0.754 (95% c.i. 0.575, 0.934), but were good predictors of cardiac death and cardiac complications, with AUC = 0.876 (95% c.i. 0.683, 1.000) and 0.840 (95% c.i. 0.659, 1.000) respectively.
NT-proBNP values 48h post op, were not good predictors of death from all causes with AUC=0.748 (95% c.i. 0.560, 0.936). However for prediction of cardiac mortality AUC was 0.907 (95% c.i. 0.807, 1.000) making it a strong predictor. For cardiac complications 48h NT-proBNP levels were very strongly predictive (Figure 9) with, AUC=0.939 (95% c.i. 0.878, 0.999).
Table 4 shows the sensitivity, specificity, ppv and npv of preoperative and postoperative NT-proBNP at predicting the outcomes. Generally, increasing the cut-off value from 40 to 90 pmol/l increases the specificity of the test, but lowers the sensitivity. The tests had a high negative predictive value, but low positive predictive value.
Table 4. The AUC, sensitivity, specificity, ppv and npv of preoperative and postoperative NT-proBNP levels in the prediction of outcomes.| Time point of | Predicted Variable | Area under the curve (AUC) | Using NT-proBNP cut-off > 40pmol/l | Using NT-proBNP cut-off > 90pmol/l | ||||||
| NT-proBNP measureent | sens | spec | ppv | npv | sens | spec | ppv | npv | ||
| Preoperative | Death | 0.83 | 73% | 80% | 31% | 96% | 55% | 92% | 46% | 94% |
| (0.673-0.993) | (46-99) | (71-88) | (13-49) | (91-100) | (25-84) | (87-98) | (19-73) | (89-99) | ||
| Cardiac death | 0.914 | 80% | 77% | 15% | 99% | 80% | 91% | 31% | 99% | |
| (0.823-1.000) | (45-100) | (68-85) | (2-29) | (96-100) | (45-100) | (85-96) | (6-56) | (97-100) | ||
| Cardiac Complications | 0.875 | 75% | 78% | 23% | 97% | 75% | 92% | 46% | 98% | |
| (0.757-0.993) | (45-100) | (70-87) | (7-39) | (94-100) | (45-100) | (87-98) | (19-73) | (95-100) | ||
| 24h postoperative | Death | 0.754 | 91% | 38% | 15% | 97% | 64% | 72% | 22% | 94% |
| (0.575-0.934) | (74-100) | (28-48) | (7-24) | (92-100) | (35-92) | (63-81) | (8-36) | (89-100) | ||
| Cardiac death | 0.876 | 100% | 37% | 8% | 100% | 80% | 71% | 13% | 99% | |
| (0.683-1.000) | (100-00) | (27-47) | (1-14) | (100-00) | (45-100) | (61-80) | (1-24) | (96-100) | ||
| Cardiac Complications | 0.84 | 88% | 37% | 11% | 97% | 75% | 72% | 19% | 97% | |
| (0.659-1.000) | (65-100) | (27-47) | (3-18) | (92-100) | (45-100) | (63-81) | (5-32) | (93-100) | ||
| 48h postoperative | Death | 0.748 | 90% | 25% | 12% | 96% | 70% | 58% | 16% | 94% |
| (0.560-0.936) | (71-100) | (16-34) | (5-19) | (87-100) | (42-98) | (48-68) | (5-27) | (88-100) | ||
| Cardiac death | 0.907 | 100% | 24% | 5% | 100% | 100% | 57% | 9% | 100% | |
| (0.807-1.000) | (100-00) | (16-33) | (0.2-10) | (100-00) | (100-00) | (47-67) | (0.6-18) | (100-00) | ||
| Cardiac Complications | 0.939 | 100% | 25% | 9% | 100% | 100% | 59% | 16% | 100% | |
| (0.876-0.999) | (100-00) | (16-34) | (3-16) | (100-00) | (100-00) | (49-69) | (5-27) | (100-00) | ||
Discussion
Emerging data from published literature indicates that preoperative measurement of BNP and NT-proBNP is a good predictor for complications after cardiac surgery 8, 11 and non-cardiac surgery.9, 12, 13, 14Patients having both cardiac and vascular surgery have high rates of cardiac disease and the role of BNP as a predictor of postoperative events in high risk cardiac patients having non-cardiac surgery has previously been described.15
This study has demonstrated that both pre-operative and postoperative measurement of NT-proBNP can help in identifying patients at high risk of major adverse events following colorectal cancer surgery. Pre-operative NT-proBNP levels may be able to predict the pre-operative cardiac status of patients but do not necessary reflect the variable dynamic sequences of postoperative stress responses which may result in adverse cardiac events. On the other hand, the postoperative measurement of NT-proBNP takes these factors into consideration, particularly with respect to the risk of cardiac death or cardiac complications.
The use of NT-proBNP as a predictive preoperative biochemical marker has significant potential clinical applications. It is envisaged that patients with high preoperative NT-proBNP levels, indicating a high risk of postoperative cardiovascular events, could be referred for cardiac optimisation. Valuable hospital resources, such as the use of intensive care monitoring, can also be targeted for patients who fall in this group. It remains to be seen whether such interventions would have any effect on patient morbidity or mortality. In our study, the greatest power of the preoperative NT-proBNP value was as a negative predictor. This means that normal NT-proBNP values were associated with low risks of cardiac events. This seems to correlate with the results found in heart failure where the European Society of Cardiology Task force guidelines for the treatment of chronic heart failure state that natriuretic peptides “may be most useful clinically as a rule out test due to consistent and very high negative predictive values.”16 A potential application of this test would be to identify patients not requiring high dependency or intensive care post-operatively from the point of view of their cardiac function, if their pre-operative NT-proBNP levels were less than 90pmol/l.
In our study, 11 patients (11%) had a rise in Tn-T post-operatively, 6 of which were not apparent clinically and 2 of which were diagnosed as silent myocardial infarctions. These 2 patients were referred to cardiologists and treated for myocardial infarction, with appropriate cardiology follow-up. The routine measurement of post operative Tn-T, although useful for these 2 patients, may not be justified in the routine care of these patients when the cost of the test is considered. However, this has not been formally assessed in a cost-benefit analysis. Previous work on higher risk patients, undergoing elective and emergency aortic aneurysm repair, has yielded much higher proportions of patients having Tn-T rises postoperatively.17 There may be more justification in routine post operative Tn-T measurement in these patients.
The study has several limitations. Firstly, it was carried out in one centre, so it may not be possible to apply the results of this study to another population because of different prevalence of cardiac disease. Secondly data on confounding factors such as intraoperative blood loss and surgical contamination was not collected in this study. These could potentially heavily influence the outcome after surgery. Remarkably, there were no anastomotic leaks diagnosed in this series of patients. It is possible that some of these cardiac complications could be attributed to undiagnosed leaks, as one previous study demonstrated that approximately 40% of patients having cardiac symptoms following a restorative colorectal resection, in fact had suffered an anastomotic leak.18
The NT-proBNP test is safe and convenient, requiring only a routine venepuncture. Currently a routine NT-proBNP test will cost the NHS £25.00 per patient and this is relatively cheap to screen some of the high-risk patients. However, there are no data to support the use of NT-proBNP in the general screening of asymptomatic populations for heart failure prior to surgery. What is clear from our study is that NT-proBNP measurements are useful as an adjunct to other clinical tools to determine the risks of patients undergoing non-cardiac surgery. With the current emerging evidence, NT-proBNP has the potential to be used in clinical practice. Patients with high risks of cardiovascular disease should have a screening NT-proBNP blood test. Patients with elevated NT-proBNP should be referred to a cardiologist for consideration of additional stress testing or echocardiogram, to assess the presence and extent of coronary artery disease. Conversely patients with normal NT-proBNP tests have the potential to avoid unnecessary patient referral for echocardiography or stress testing.
References
- 1.Bokey E L, Chapuis P H, Fung C, Hughes W J, Koorey S G et al. (1995) Postoperative morbidity and mortality following resection of the colon and rectum for cancer. Diseases of the Colon & Rectum. 38(5), 480-6.
- 2.Eagle K A, Berger P B, Calkins H, Chaitman B R, Ewy G A et al. (2002) ACC/AHA Guideline Update for Perioperative Cardiovascular Evaluation for Noncardiac Surgery--Executive Summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the1996Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery).[see comment]. Anesthesia & Analgesia. 94(5), 1052-64.
- 3.Doust J A, Pietrzak E, Dobson A, Glasziou P. (2005) How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: systematic review.[see comment]. , Bmj 330(7492), 19.
- 4.Lee T H, Marcantonio E R, Mangione C M, Thomas E J, Polanczyk C A et al. (1999) Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 100(10), 1043-9.
- 5.Goldman L, Caldera D L, Nussbaum S R, Southwick F S, Krogstad D et al. (1977) Multifactorial index of cardiac risk in noncardiac surgical procedures. , New England Journal of Medicine 297(16), 845-50.
- 6.Gibson S C, Payne C J, Byrne D S, Berry C, Dargie H J et al. (2007) B-type natriuretic peptide predicts cardiac morbidity and mortality after major surgery. , British Journal of Surgery 94(7), 903-9.
- 7.Vuolteenaho O, Ala-Kopsala M, Ruskoaho H. (2005) BNP as a biomarker in heart disease. Advances in Clinical Chemistry 40, 1-36.
- 8.Eliasdottir S B, Klemenzson G, Torfason B, Valsson F. (2008) Brain natriuretic peptide is a good predictor for outcome in cardiac surgery. Acta Anaesthesiologica Scandinavica. 52(2), 182-7.
- 9.Feringa H H, Bax J J, Elhendy A, R de Jonge, Lindemans J et al. (2006) Association of plasma N-terminal pro-B-type natriuretic peptide with postoperative cardiac events in patients undergoing surgery for abdominal aortic aneurysm or leg bypass. , American Journal of Cardiology 98(1), 111-5.
- 10.Yeh H M, Lau H P, Lin J M, Sun W Z, Wang M J et al. (2005) Preoperative plasma N-terminal pro-brain natriuretic peptide as a marker of cardiac risk in patients undergoing elective non-cardiac surgery.[see comment]. , British Journal of Surgery 92(8), 1041-5.
- 11.Hutfless R, Kazanegra R, Madani M, Bhalla M A, Tulua-Tata A et al. (2004) Utility of B-type natriuretic peptide in predicting postoperative complications and outcomes in patients undergoing heart surgery. , Journal of the American College of Cardiology 43(10), 1873-9.
- 12.Mahla E, Baumann A, Rehak P, Watzinger N, Vicenzi M N et al. (2007) N-terminal pro-brain natriuretic peptide identifies patients at high risk for adverse cardiac outcome after vascular surgery.[see comment]. Anesthesiology. 106(6), 1088-95.
- 13.Rajagopalan S, Croal B L, Bachoo P, Hillis G S, Cuthbertson B H et al. (2008) N-terminal pro B-type natriuretic peptide is an independent predictor of postoperative myocardial injury in patients undergoing major vascular surgery. , Journal of Vascular Surgery 48(4), 912-7.
- 14.Rodseth R N, Padayachee L, Biccard B M. (2008) A meta-analysis of the utility of pre-operative brain natriuretic peptide in predicting early and intermediate-term mortality and major adverse cardiac events in vascular surgical patients. Anaesthesia. 63(11), 1226-33.
- 15.Leibowitz D, Planer D, Rott D, Elitzur Y, Chajek-Shaul T et al. (2008) Brain natriuretic peptide levels predict perioperative events in cardiac patients undergoing noncardiac surgery: a prospective study. Cardiology. 110(4), 266-70.
- 16.Remme W J, Swedberg K. (2002) European Society of C. Comprehensive guidelines for the diagnosis and treatment of chronic heart failure. Task force for the diagnosis and treatment of chronic heart failure of the European Society of Cardiology. , European Journal of Heart Failure 4(1), 11-22.
Cited by (1)
This article has been cited by 1 scholarly work according to:
Citing Articles:
Journal of Onco-Anaesthesiology and Perioperative Medicine (2025) Crossref
V. Naik, Harini Narayanan - Journal of Onco-Anaesthesiology and Perioperative Medicine (2025) Semantic Scholar
