Photobiomodulation, Depression, Anxiety, and Cognition
Abstract
Background
Anxiety and depression are key barriers to healthy aging and greatly heighten the risk for many negative health issues that seriously impact life quality.
Aim
This mini review examines the potential of low level laser treatments or photobiomodulation therapy for ameliorating severe anxiety and depression in older adults.
Methods and Procedures
Articles that adressed the current topic of interest extracted from PUBMED and Google Scholar were carefully and presented in narrative form.
Results
Photobiomodulation therapy appears to be a safe efficacious modality for ameliorating various degrees of anxiety and depression and for improving cognition, and is supported by several well established mechanisms of action at the molecular, cellular, and tissue levels.
Conclusion
More research to examine who might benefit most from this form of therapy, and in what respect in this area of growing global concern and few intervention options is strongly warranted.
Author Contributions
Copyright © 2021 Ray Marks
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Depression among the elderly is now considered among the leading and most disabling health challenges facing the older population, and will be the foremost disabler by 2030 1, 2. However, its management and current treatments offer many challenges, and have many limitations 3, 4, 5. Anxiety, the most common mental health concern among older adults 6, and one often associated with depression, is also a common debilitating state of fears that commonly impacts health behaviors negatively and significantly. Among the various strategies for intervening in this regard, a form of low level laser known as photo biomodulation therapy or PBM, which can be applied transcranially and that appears to safely activate selected brain pathways and tissues involved in mood disturbances, has been advocated for some time 7, 8, 9, 10.
This does not negate other forms of intervention that do exist, but is studied because it may fill a gap in areas where these more mainstream interventions do not help to directly alleviate the highly negative impact of various forms of persistent anxiety, which often accompanies depression, nor pathways inducing associated feelings of sadness, helplessness, loss of interest in self-care as well as pleasure in daily activities in a practical as well as possibly in an observable functional and neural context 10. On the other hand, multiple studies support the idea that the perpetuation of unrelieved states of suffering, including feelings of hopelessness, and low self-worth, may in turn, increase or produce unwanted stress and frustration levels, while adversely impacting coping ability, sleep, energy levels, and appetite, as well as serving as a risk factor for bone loss and osteoporotic fractures 11, as well as cardiovascular disease 12. In contrast, transcranial photobiomodulation TPBM light energy applications, which commonly involve the delivery of various forms of low level red light spectra via the skull to the brain, appears to have direct effects on brain tissue physiology thought to underpin depression, such as inflammation 13 that may help to alleviate the immense suffering experienced by the chronically anxious and/or depressed older individual, while affording them a heightened sense of emotional control, plus a sense of optimism about possible changes that might yet occur with the steady application of one or more forms of therapy over time. This use of nonthermal levels of visible or near infrared light for treating depression and anxiety in turn, may be expected to not only mediate the biology and pathways related to the risk and progression of these conditions via photochemical mechanisms 10, 13, but may also indirectly prevent the onset of, or reduce the risk of acquiring any excess or secondary chronic illness burden, injurious tissue degeneration or damage, and/or other adverse life events and losses, including mobility losses and falls associated with aging that often in turn, heighten depression and anxiety 11, 14. In addition, there may be fewer social disruptions, along with fewer associated medical visits. At the same time, self-management practices may be more readily accomplished, adhered to, and effective. On the other hand, a failure to alleviate protracted unrelenting bouts of anxiety and depression, may foster excess pain experiences, and possible substance abuse, along with a greater likelihood of premature death, higher rates of inflammation, blood pressure issues, memory challenges, and a decreased desire for physical activities often recommended for intervening on depression and anxiety 15.
In light of the severe impact of excessive anxiety and depression as mentioned above, plus its detrimental impact on motivation, as well as health seeking and promoting behaviors, and that evidence shows many factors underpinning depression and anxiety are amenable to therapy and prevention 13, this mini review elected to selectively focus on the known benefits of applying photo biomodulation therapy in the context of anxiety, depression, and possible memory challenges in older adults that might serve to place the individual in a more salient stage of ‘preparedness’ to partake in self-care and be responsive to other forms of non-pharmacologic therapy given the lack of safe forms of practical intervention to ameliorate these conditions in this regard. While other modes of intervention such as meditation may be helpful in this respect, it is possible that some cases of severe chronic mood conditions need to be overcome first by more direct interventions such as those produced by TPBM. Since quality of life may be severely jeopardized by chronic mood disorders, as well as cognitive challenges that may be reversible, it was believed line of research would prove fruitful to examine.
Materials and Methods
To attain the aims of this review, we attempted to locate salient data housed on PUBMED and GOOGLE SCHOLAR using the key terms, transcranialphotobiomodulation/lower level laser therapy and depression/anxiety/older adults. All forms of publication were deemed acceptable if they addressed the topics of interest noted above and there were no yearly or methodological restrictions. The most salient articles related to the transcranial use of photobiomodulation therapy, rather than systemic approaches, were duly examined and those that were noteworthy are presented in narrative form. All modes of application employed in the various research studies were accepted as valid, as were all definitions of anxiety and depression. Moreover, since the article was designed to serve as a general one to introduce the topic, rather than a systematic review, it did not consider any of the currently reported research endeavors in depth, but rather the goals was to present a snapshot of the prevailing trends in this realm and the potential of this modality for clinical purposes. As per Hamblin 10, 16, the term photobiomodulation, which refers to the use of red or near-infrared light to stimulate, heal, regenerate, and protect tissues was used predominantly in this brief review. Also termed low level laser light or therapy in the past, as well as simply photobiomodulation to describe the therapeutic process these technical terms are used interchangeably in this report. For a succinct review of recent controlled clinical trials, the articles by de Oliviera Foncesca et al. 15, Askalsky and Iosifescu 3 and Hamblin 10, 16 are recommended.
Search Results
General Observations
Depressive and anxiety disorders have been shown to be associated with premature or advanced biological aging and consequently to adversely impact life quality adversely, as well as somatic health 17. Treatments with antidepressant medication or running therapy, however, found to be effective for many with mood and anxiety disorders 17, are unlikely to be safe in all respects, for example, if the individual is frail 18, or they have a high falls risk profile, or if the medications employed produce unwanted side effects, such as obesity. As well, existing antidepressants not only have burdensome side effects, but are only partially effective in many cases, and relapse is frequently observed 3. For vulnerable older adults who cannot exercise readily and do not respond favorably to antidepressant medications, it appears that non-thermal non-invasive applications of visible or near infrared light transcranial neuro-stimulation may be able to stimulate or inhibit targeted biological cells and tissues that undermine emotional health via a reproducible photochemical mechanism 10, 16.
Indeed, since poorly treated anxiety and depression can cause immense suffering, family disruptions, and disability, while worsening the outcomes of many medical illnesses, and/or increasing mortality rates, it appears very important to be able to offer vulnerable older adults a minimally invasive and safe possible therapeutic option 19. It is increasingly essential as well to consider that poorly treated depression or anxiety or both can be expected to increase the risk for comorbid diseases, negative inflammatory responses, negative cognitions, health behaviors, and negative immunity associated changes 20.
On the other hand, if an individual who has been severely immobilized by their depression or anxiety symptoms can experience some relief in a short time frame from repeated bout of photo biomodulation therapy that may be accompanied by important cognitive improvements, they may be more readily motivated towards pursuing physical activity and other recommended self-help approaches.
What the Research on Photobiomodulation Shows
For over 20 years, and despite their varied modes of research and photobiomodulation application strategies, most published data support the utility of this form of therapy for reversing or reducing the severity of anxiety and depression. In addition, several mechanism of action have been affirmed in multiple studies for both those that influence depression as well as anxiety 21, 22.
In addition to the findings of positive behavioral effects of chronically stimulating rats using cortical infra red stimulation, plus favorable neurogenic cortical hippocampus tissue changes 23, one controlled clinical trial similarly observed that low level laser applications were indeed able to enhance the effects of cognitive training approaches applied to depressed subjects 24. Another 25, showed that while participants generally reported more positive affective states than negative, overall affect improved significantly in the treated group when compared to the placebo control group. These data were taken to imply that transcranial laser stimulation is a potentially useful non-invasive and efficacious approach for purposes of fostering brain functions such as those related to the cognitive and emotional dimensions. Moreover, the mode of application may be manipulated to foster differential outcomes, with some more profound than others 26, or effects comparable to more time consuming interventions as far as anxiety is concerned 27.
Shiffler et al. 8 further showed post stimulation psychological benefits two and four weeks following but a single treatment of near infrared light applied to the forehead in a pilot study of 10 patients with major depression and anxiety. Indeed, in this first study to examine major depressive disorder patients, normally a fairly intractable condition, both the depression and anxiety symptoms experienced previously by the participants were readily alleviated at two weeks post-irradiation. At the end of four weeks, 6/10 patients experienced a remission in their depression and 7/10 experienced remission of their anxiety.
In the study by Tanaka et al. 23 who evaluated the antidepressant and anxiolytic effects of infrared radiation in a randomized controlled trial using an experimental animal model, this group similarly found chronic infrared radiation exposure tended to decrease the indicators of depression as well as anxiety-like behavior employed in the study. As well, selected histological assays of the hippocampus showed favorable responses in both acutely and chronically exposed infrared radiation groups compared to the tissue samples of the control group. These results were taken to indicate that chronic infrared radiation may be able to produce comparable antidepressant- and anxiolytic-like effects in the human situation.
Other findings relative to anxiety benefits are cited by Brochado et al. 27 and Yang et al. 28 and tend to echo and provide further support for the efficacy of photo biomodulation stimulation effects for mitigating chronic anxiety states. In addition, Gabel et al. 29 who applied photo biomodulation to the back and thighs as an adjunct to physical therapy for chronic pain, also found the patients experienced improvements in concurrent depression. Kerppers et al. 30 too, who studied the use of TPBM found this mode of intervention to decrease anxiety and depression, as well as increasing brain activity as a whole. Using an animal model of depression, Mohammed 31 similarly found laser irradiation to successfully ameliorate depression induced by reserpine, which was deemed indicative of the potentially beneficial anti-depressant effects of low-level infrared laser irradiation on tissues associated with depression in normal and healthy animal brain tissues.
In addition, TPBM appears to enhance frontal lobe cognitive activity 33, 34, as well as improving neuron metabolic capacity. As well, when examined independently in depressed humans, or in combination with coenzyme Q10, this approach appears to reduce oxidative stress, neuro-inflammation, and cell death associated with depression 35. Alone or in combination with other interventions, TPBM may hence prove very helpful clinically for ameliorating the severity of symptoms in selected cases of major depression or reactive depression, among other cognitive impairments experienced at high rates among the elderly.
According to dos Santos Cardosa 36 TPBM also has the potential to improve brain energy metabolism as well helping to control damaging inflammatory processes found to prevail among the aged and that contributes to their oftentimes declining cognitive brain functions. Accordingly, studies in humans have specifically shown that this form of therapy does tend to improve electrophysiological brain response activity and cognitive functions such as attention, learning, memory and mood among older adults.
Importantly, too, Cassano et al. 37, who investigated the tolerability and efficacy of near infrared applications in selected cases diagnosed as having major depression found those who received this form of treatment appeared to tolerate this well without any serious adverse events. Other data show low level infra red rays applied to the frontal region of the skull in depressed and anxious adults may not only help to reverse neurotransmitter imbalances, but may foster cerebral blood flow and metabolic processes in different areas of the brain-found deficient in depressed elders 38, such as the frontal lobe 39. Photo biomodulation also appears to improve any present mitochondrial dysfunction, as well as oxidative stress mechanisms and neuroinflammation. Improvements in any impaired neurogenesis functions (i.e., ability to regenerate and/or grow nerves/neurons); are other explanations for its efficacy.
These post stimulation consistently observed increases in regional blood flow in the brain of depressed individuals subjected to TPBM and others may thus augment cerebral energy metabolism, a contributing factor to depressive manifestations 40, while their apparent antidepressant effect coupled with the enhanced blood flow in turn, potentially contributes to the increased chances of the patient experiencing some degree of recovery from persistent mood disorders and impaired cognitions 36, 40.
It is also known that red light therapy can foster the release of nitric oxide, a vasodilator, that could help improve circulation to selectively irradiated cortical areas, while near infra red light spectra may help to specifically activate antioxidant mechanisms that reduce damaging oxidative stresses. According to Xu et al. 41 depression like behaviors can also be reduced in response to photobiomodulation applications given their observed ability to impact on neurotransmitter abnormalities and promote mitochondrial function in the prefrontal cortex. According to Xu et al. 41, red light therapy also stimulates neurogenesis and synaptogeneisis and protects against cell death by improving levels of brain-derived neurotrophic factor. As indicated in multiple, studies conducted in different animal models and in humans, TPBM appears to not only have the power to improve cerebral metabolic activity as well as blood flow 42, and ATP production, but to also enhance anti-inflammatory and antioxidant pathway influences, which are known to prevail in the context of various degrees of depression and distress 3, 9.
The application of the TPBM is hence not only a promising approach for the treatment of a wide range of neuropsychiatric disorders, including disorders characterized by poor regulation of emotion such as major depressive disorder 33, 35, 40, 43, 44, 45, but the clear demonstration of the multiple relevant mechanisms of action explaining its observed impact on cerebral cortical tissues and cells, greatly strengthen the credibility of the current therapeutic observations 16. Moreover, this is seen to occur regardless of method of stimulation and target tissues examined, and even though the techniques of application vary, they all essentially direct light, typically in the near infra red range of the spectrum to the brain through the skull, where they appear to readily activate numerous desirable cellular, circulatory, and anti-inflammatory processes. There are hence currently a wide range of related clinical trials in this promising realm, including those targeting major depressive disorder, generalized anxiety disorder, dementia, traumatic brain injury and post-traumatic stress disorder to support its more widespread usage and utility 7, 10, 16, 43, 44, 45.
As well, new methods of application, such as those that utilize an intranasal mode have become an attractive and potentially useful option for the treatment of a variety of potentially reversible brain conditions because evidence to date shows that nostril-based applications can improve blood rheology, and cerebral blood flow, that may produce results equivalent to those observed when using peripheral intravenous laser irradiation procedures 46. Theoretically, these light rays can also be expected to stimulate cortical mitochondrial respiratory chain components, as well as significantly increasing cerebral blood flow 3, 42 and neurogenesis 47. Its anti-apoptotic, anti-inflammatory, and antioxidative responses, may also provide for pain relief, often a key contributor to the presence of persistent anxiety and depressive states. Xioran et al. 48 also highlights the promise of various forms of light therapy for potentially improving brain activity patterns in those diseases or situations affected by brain dysfunction and/or injury and that may engender depression and anxiety states. In addition, Salgado et al. 42 report transcranial low level light therapy applied with an LED device (light-emitting diode device—627 nm, 70 mW/cm2, 10 J/cm2, for a total of 2 minutes) to the frontal and parietal encephalic regions of elderly individuals, twice weekly for 4 weeks, increased blood flow velocity in the middle and basilar cerebral arteries. This suggested that the procedure might prove to be a useful form of prophylactic therapy in the elderly population, who are commonly affected by age associated vascular and cognitive alterations often found in cases with chronic depression and as supported by Gutiérrez-Menéndez et al. 45. It may also enhance excitatory synaptic transmission 50, despite the presence of any already apparently compromised integrity of the frontal-limbic networks implicated in depression, as well as frequent observations of volumetric hippocampus, anterior cingulate cortex, prefrontal cortex, striatum, and amygdale reductions, as well as compromised white matter integrity 51, and the favorable effects can potentially be sustained with bilateral prefrontal sited applications delivered intermittently over time 45.
In sum, as discussed by Urquhart et al. 52 photobiomodulation applications of low-power, high-fluence light in the red to near-infrared range (usually between 630-1100 nm) are found to modulate cortical mitochondrial respiratory pathways and other salient neural mechanisms implicated in depression and anxiety among the elderly in a non-destructive and non-thermal manner. While enhancing cerebral oxygenation and cognitive function, among other positive attributes including metabolic and hemodynamic alterations in the brain, it appears photobiomoduation applications can activate key neuroprotective mechanisms, while enhancing cognitions. Although initially viewed quite skeptically for some time 10, 16, multiple current reviews and studies by various groups tend to support this form of therapy as consistently promising and helpful in safely alleviating depression, anxiety, and cognitive dysfunction. It also appears that TPBM as applied to alleviating intractable bouts of depression and anxiety may also reduce the extent of any persistent mood states through its positive influence on pain, wound healing, muscle function, and aesthetic applications 15.
Discussion
Depression and anxiety, major health issues impacting older adults negatively and significantly remain extremely challenging to eliminate. This review discusses findings concerning the possible role of photobiomodulation, a form of light therapy that utilizes non-ionizing light sources, including lasers, light emitting diodes, or broadband light to treat brain tissues, while providing a safe means of modulating brain activity without any irreversible damage in this regard 48. According to Gutiérrez-Menéndez et al. 45 and an increasing number of researchers 16, photobiomodulation, a non invasive brain modulation technique that can be applied in different formats, shows considerable promise in this regard for being able to stimulate, preserve and regenerate cells and tissues, including mitochondrial photon absorption, function, and integrity, while activating signaling pathways, transcription factors and protective genes, and anti-inflammatory mechanisms 47, 53 associated with depressive symptoms and others 7.
Figure 1.Schematic of hypothesized benefits that may accrue from applications of transcranial photobiomodulation TPBM to cases suffering from protracted anxiety and/or depression plus cognitive dysfunction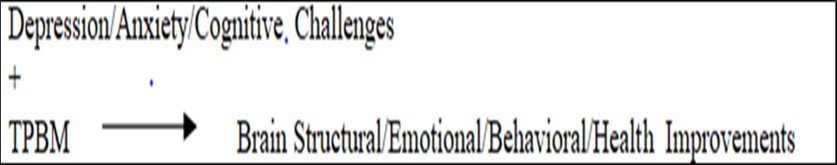
Older adults were the specific focus in this review, given the high prevalence rates of mood disorders in this group, including those with Alzheimer’s disease 47, which may worsen with unrelieved albeit preventable depression symptoms. A high number of depressed older adults with memory loss may not be amenable to psychotherapy or alternate mainstream forms of therapy, such as exercise. As well, as opposed to pharmacotherapy, which may only have a limited impact in severe cases, Disner et al. 24 note low-level light therapy with transcranial laser is a non-invasive form of therapy that can be applied selectively to the prefrontal lobe to reduce depression and anxiety symptoms through its ability to foster a state of potentially sustainable neuro enhancement 45. Additional research further shows features of depression, including impaired neuronal metabolism, chronic pain, and various degrees of cognition, may indeed be modified favorably by this approach.
Kerppers et al 30 -who examined transcranial photobiomodulation in an effort to heighten neural activity in anxious and/or depressed younger subjects did find this modality was able to stimulate brain activity. This was also the view of Maiello et al. 22 and Cassano et al. 44. Moreover, the fact that red and near infra red light stimuli can be selectively modulated and adjusted non invasively to effect cognitive targets associated with declines in emotional health and impaired psychological status 54 is expected to help minimize or reduce the complex challenges of excess distress attributable to mood disturbances and their oftentimes disabling immobilizing ramifications and negative health consequences 16. Indeed, numerous studies that do exist all tend to show that in agreement with the known structural and dysfunctional alterations of the brain in depression and anxiety states, this non invasive form of light stimulation does consistently appear to mitigate various degrees of mood disturbances, effectively and significantly, and can reverse abnormalities, including those associated with severe depression states, as well as cognitions deemed irreversible. In addition, these improvements can be explained by observable related changes in one or more brain sites, molecular pathways, and neural processes implicated in mediating one or both of these disabling psychological conditions 43. These include, but are not limited to favorable impacts on mitochondrial metabolism and other pathways relevant to major depressive disorders. In addition, studies on animal models indicate the benefits from this form of therapy appear to be comparable to those achieved by antidepressant medications. Clinical studies also indicate good tolerability.
Taken as a whole, and even if studies to the contrary have not been published, in accord with Hamblin 10, 16 and others eg.55, photo biomodulation, a novel form of light therapy that utilizes non-ionizing light sources, including lasers, light emitting diodes, or broadband light, does appear to be a highly promising safe means of modulating brain cortical activity in simulated as well as clinical depression and anxiety without any observable damage when delivered transcranially 43. Also associated with cognitive improvements, memory, and behavioral improvements, including attenuation of depression and anxiety, and increased cortical oxygenation, the application of TPBM may be especially helpful for alleviating suffering in older adults who cannot exercise readily, take medications, or interact effectively clinically or in a group 55, especially those with cognitive challenges and frail elders with multiple morbidities. Thus future work to validate these preliminary findings, as well as clarifying the apparent clinical value of TPBM for larger more diverse samples that may lead to more targeted and successful therapies is strongly warranted. As well, the role of TPBM as an adjunctive therapeutic tool should be examined. In the interim, since many current intervention approaches, it appears that subject to careful patient evaluation concerning the nature and etiology of any prevailing chronic mood disturbances, the carefully construed and monitored application of TPBM can be expected to safely reduce feelings of excess anxiety 56 and depression 45 to some degree, with minimal risk, regardless of age and extent of the severity of one or more mood disturbances. To shed more light on the potential for TPBM and its implications on health status as a whole, testing whether such an application yield important parallel improvements in parameters related to the function of the musculoskeletal and cardiorespiratory systems, plus the immune system will be valuable. Whether bone health, the degree of sleep and life quality, and the extent of premature or biological aging attributable to inflammation can be attenuated is also of possible value to ascertain 17, 55, 57 and may be highly informative. Moreover, identifying whether targeted and repeated TPBM applications can foster a stronger desire among patients towards self care and other positive behaviors, as well as a greater ability to adhere to health recommendations and to feel efficacious in achieving favorable health and active aging outcomes in the short and long-term time periods could prove invaluable.
In the interim, and in line with growing evidence from multiple sources, the transcranial application of diverse forms of delivering low level laser light therapy to the prefrontal cotical region of depressed animals and humans appears to offer a consistently efficacious result as far as producing measureable favorable organic changes in the stimulated neural tissues and structures that are vital to emotional regulation and wellbeing. Furthermore, and importantly, the currently demonstrated benefits of TPBM may be expected to heighten favorable outcome expectations and thus more positive perspectives for many older adults-in general, especially in light of the unfavorable stance often accompanying the stigma of depression and anxiety, in addition to widespread ageism issues and perspectives, plus vulnerability to the use of psychotropic drugs. To further affirm and advance its clinical value, however, more comparative studies, as well as dose response and other studies assessing the degree to which TPBM can act as an effective approach for enhancing mainstream intervention approaches such as exercise, counseling, pharmacologic and stress control approaches may be insightful. Finally, in terms of cost benefit analyses, it appears the low monetary and energy costs of TPBM, along with its ease of usage might be better exploited in terms of its possible value for reducing the immense degree of suffering, as well as unwanted consequences of depression, such as cardiovascular disease 58, and more recently COVID-19, among the growing older adult population, if more clinical evidence from long-term prospective studies of various degrees of distress in healthy and chronically impaired older adults are forthcoming.
Indeed, by providing hope to many, as opposed to despair, along with cost savings to elder care organizations, health policy makers, and governmental agencies, the apparent merits of TPBM should be studied sooner rather than later by all those in the health field who seek to advance elder care and raise older adults life quality, while preventing undue suffering and emotional pain in a cost-effective and safe manner.
Attributes or factors and parameters that may impact or influence efficacy and outcomes in clinical and preclinical studies of TPBM that should be carefully examined in light of their possible differential effects on the quantity of light absorbed, and hence on the desired outcomes include:
the degree of prevailing irradiance
treatment timing and repetition
pulse attributes and wavelength/light color
the degree of fluence
power density effects
Other mediating or moderating factors that can be examined to gain further insight into the efficacy of TPBM for intervening in depression and anxiety are the characteristics of the subject, and application site s, the methods of applying the light stimuli, and the prevailing degree of emotional and neural dysfunction 10, 15, 16, 59, 60. Others not well studied to date are the role of: 1) caregiver empathy and knowledge; 2) patient attributes and beliefs; 3) general health status; 4) living conditions; 5) social support; 6) degree of follow up evaluations.
Successful results may also depend on the ability of the provider to personalize any recommended phototherapy application, as well as follow up plans and timely carefully construed evaluations.
In the meantime, the work to date not only embodies, but is consistent with the contemporary paradigm shift away from dysregulation of single neurotransmitter systems in cases of depression towards circuit level abnormalities impacting function across multiple brain regions and neurotransmitter systems that is comparable to the actions of antidepressant medications 43, 54, as well as efforts to foster successful aging. Combining transcranially induced light therapy alongside antidepressant and/or other medications and educational approaches can also be expected to help speed up the rate at which possible beneficial outcomes are realized. Moreover, those treated optimally will undoubtedly tend to experience better overall health status, sleep quality, and a higher life quality than those who do not – all things considered 2, 61 62.
In this regard, although ignored for many years, it appears hard to refute the idea that TPBM is a potentially effective, sustainable, safe, and compatible intervention mode for purposes of offsetting the immense suffering attributable to the presence and risk of multiple cognitive and health challenges faced by many elderly, if not all. Its optimal value too, which may yet be untapped, appears to merit considerable attention in this regard, and is strongly encouraged.
Conclusions
Transcranial
photobiomodulation therapy, a novel non-invasive form of neuromodulatory stimulation is emerging as a viable adjunct to alleviating the disabling cognitive states of anxiety and depressive, highly prevalent among the elderly.
Demonstrated to minimize depression and anxiety symptoms favorably and safely and with good tolerability and on the basis of multiple empirically derived mechanisms of impact, the approach seems highly promising for fostering more optimal healthy aging and personalized care in many respects.
More research to carefully examine how this strategy can be optimized for both prophylactic as well as therapeutic purposes and who will benefit and why will hence likely prove highly fruitful for countering this growing burdensome mental health epidemic among older adults, but its present application, where indicated, which is engendering positive results on a consistent bases, should not be overlooked.
References
- 2.Blazer D G. (2003) Depression in late life: review and commentary. , J Gerontol A Biol Sci Med Sci 58(3), 249-265.
- 3.Askalsky P, Iosifescu D V. (2019) Transcranial photobiomodulation for the management of depression: current perspectives. , Neuropsychiatr Dis Treat 22(15), 3255-3272.
- 4.Zis P, Daskalaki A, Bountouni I, Sykioti P, Varrassi G. (2017) Depression and chronic pain in the elderly: links and management challenges. , Clin Interv Aging 21(12), 709-720.
- 5.Mitchell P B, Harvey S B. (2014) Depression and the older medical patient--when and how to intervene. , Maturitas 79(2), 153-9.
- 7.Hennessy M, Hamblin M R. (2017) Photobiomodulation and the brain: a new paradigm. , J Opt 19(1), 013003.
- 8.Schiffer F, Johnston A L, Ravichandran C, Polcari A, Teicher M H. (2009) Psychological benefits 2 and 4 weeks after a single treatment with near infrared light to the forehead: a pilot study of 10 patients with major depression and anxiety. , Behav Brain Funct 5, 46.
- 9.Salehpour F, Mahmoudi J, Kamari F, Sadigh- Eteghad S, Rasta S H. (2018) Brain photobiomodulation therapy: a narrative review. , Mol Neurobiol 55(8), 6601-6636.
- 10.Hamblin M R. (2016) Shining light on the head: photobiomodulation for brain disorders. , BBA Clin 6, 113-124.
- 11.Zhou J, Xue Y. (2020) Depression, falls, and osteoporotic fractures. , Osteoporos Int 31(6), 1175.
- 12.Raič M. (2017) Depression and heart diseases: leading health problems. , Psychiatr Danub 29(4), 770-777.
- 13.Berk M, Williams L J, Jacka F N, O'Neil A, Pasco J A. (2013) So depression is an inflammatory disease, but where does the inflammation come from?. , BMC Med 11, 200.
- 14.Iaboni A, Flint A J. (2013) The complex interplay of depression and falls in older adults: a clinical review. , Am J Geriatr Psychiatry 21(5), 484-92.
- 15.de Oliveira LDSSCB, Souza E C, RAS Rodrigues, Fett C A, Piva A B. (2019) The effects of physical activity on anxiety, depression, and quality of life in elderly people living in the community. Trends Psychiatry Psychother. 41(1), 36-42.
- 16.Hamblin M R. (2016) Photobiomodulation or low-level laser therapy. , J Biophotonics.9(11-12): 1122-1124.
- 17.Lever-van Milligen BA, Verhoeven J E, Schmaal L, van Velzen LS, Révész D. (2019) The impact of depression and anxiety treatment on biological aging and metabolic stress: study protocol of the MOod treatment with antidepressants or running (MOTAR) study. , BMC Psychiatry 19(1), 425.
- 18.Vaughan L, Corbin A L, Goveas J S. (2015) Depression and frailty in later life: a systematic review. , Clin Interv Aging 10, 1947-58.
- 19.Casey D A. (2017) Depression in older adults: a treatable medical condition. , Prim Care 44(3), 499-510.
- 20.Morimoto S S, Alexopoulos G S. (2011) Immunity, aging, and geriatric depression. , Psychiatr Clin North Am 34(2), 437-49.
- 21.Eshaghi E, Sadigh-Eteghad S, Mohaddes G, Rasta S H. (2019) Transcranial photobiomodulation prevents anxiety and depression via changing serotonin and nitric oxide levels in brain of depression model mice: A study of three different doses of 810 laser. Lasers Surg Med. 51(7), 634-642.
- 22.Maiello M, Losiewicz O M, Bui E, Spera V, Hamblin M R. (2019) Transcranial Photobiomodulation with near-infrared light for generalized anxiety disorder: a pilot study. Photobiomodul Photomed Laser Surg. 37(10), 644-650.
- 23.Tanaka Y, Akiyoshi J, Kawahara Y, Ishitobi Y, Hatano K. (2010) Infrared radiation has potential antidepressant and anxiolytic effects in animal model of depression and anxiety. , Brain Stimul 4(2), 71-6.
- 24.Disner S G, Beevers C G, Gonzalez-Lima F. (2016) Transcranial laser stimulation as neuroenhancement for attention bias modification in adults with elevated depression symptoms. , Brain Stimul 9(5), 780-787.
- 25.Barrett D W, Gonzalez-Lima F. (2013) Transcranial infrared laser stimulation produces beneficial cognitive and emotional effects in humans. , Neuroscience 230, 13-23.
- 26.Henderson T A, Morries L D. (2017) Multi-watt near-infrared phototherapy for the treatment of comorbid depression: an open-label single-arm study. Front Psychiatry. 8, 187.
- 27.Brochado F T, Jesus L H, Carrard V C, Freddo A L, Chaves K D. (2018) Comparative effectiveness of photobiomodulation and manual therapy alone or combined in TMD patients: a randomized clinical trial. Braz Oral Res. 32, 50.
- 28.Yang L, Wu C, Tucker L, Dong Y, Li Y. (2021) Photobiomodulation therapy attenuates anxious-depressive-like behavior in the TgF344 rat model. J Alzheimers Dis.
- 29.Gabel C P, Petrie S R, Mischoulon D, Hamblin M R, Yeung A. (2018) Case control series for the effect of photobiomodulation in patients with low back pain and concurrent depression. Laser Ther. 27(3), 167-173.
- 30.Kerppers F K, Dos Santos KMMG, MER Cordeiro, MC da Silva Pereira, Barbosa D. (2020) Study of transcranial photobiomodulation at 945-nm wavelength: anxiety and depression. Lasers Med Sci. 35(9), 1945-1954.
- 31.Mohammed H S. (2016) Transcranial low-level infrared laser irradiation ameliorates depression induced by reserpine in rats. , Lasers Med Sci 31(8), 1651-1656.
- 32.Chan A S, Lee T L, Yeung M K, Hamblin M R. (2019) Photobiomodulation improves the frontal cognitive function of older adults. , Int J Geriatric Psychiatry 34(2), 369-377.
- 33.Salehpour F, Rasta S H. (2017) The potential of transcranial photobiomodulation therapy for treatment of major depressive disorder. , Rev Neurosci 28(4), 441-453.
- 34.Salehpour F, Farajdokht F, Cassano P, Sadigh-Eteghad S, Erfani M. (2018) Near-infrared photobiomodulation combined with coenzyme Q10 for depression in a mouse model of restraint stress: reduction in oxidative stress, neuro inflammation, and apoptosis. , Brain Res Bull 144, 213-222.
- 35.Cassano P, Petrie S R, Hamblin M R, Henderson T A, Iosifescu D V. (2016) Review of transcranial photobiomodulation for major depressive disorder: targeting brain metabolism, inflammation, oxidative stress, and neurogenesis. , Neurophotonics 3(3), 031404.
- 36.F dos Santos Cardoso, Gonzalez-Lima F, da Silva SG. (2021) Photobiomodulation for the aging brain. Ageing Res Rev. , Jul 26, 101415.
- 37.Cassano P, Cusin C, Mischoulon D, Hamblin M R, L De Taboada. (2015) Near-infrared transcranial radiation for major depressive disorder: proof of concept study. , Psychiatry 352979.
- 38.Matsuo K, Kato T, Fukuda M, Kato N. (2000) Alteration of hemoglobin oxygenation in the frontal region in elderly depressed patients as measured by near-infrared spectroscopy. , J Neuropsychiatry Clin Neurosci 12(4), 465-471.
- 39.Fonseca M O, Soares C P, Joaquim R M, Veras A B. (2019) Transcranial photobiomodulation in the treatment of major depression. , Clin Psychiatry 5(1), 1.
- 40.Cao X, Li L P, Wang Q, Wu Q, Hu H H. (2013) Astrocyte-derived ATP modulates depressive-like behaviors. , Nat Med 19(6), 773-777.
- 41.Xu Z, Guo X, Yang Y, Tucker D, Lu Y. (2017) Low-level laser irradiation improves depression-like behaviors in mice. , Mol Neurobiol 54(6), 4551-4559.
- 42.ASI Salgado, Cidral-Filho F J, Martins D F, Kerppers Parreira RB. (2019) Cerebral blood flow in the elderly: impact of photobiomodulation. In Photobiomodulation in the Brain 473-477.
- 43.Caldieraro M A, Cassano P. (2019) Transcranial and systemic photobiomodulation for major depressive disorder: A systematic review of efficacy, tolerability and biological mechanisms. , J Affect Disord 243, 262-273.
- 44.Cassano P, Petrie S R, Mischoulon D, Cusin C, Katnani H. (2018) Transcranial Photobiomodulation for the treatment of major depressive disorder. the ELATED-2 pilot trial. Photomed Laser Surg. 36(12), 634-646.
- 45.Gutiérrez-Menéndez A, Marcos-Nistal M, Méndez M, Arias J L. (2020) Photobiomodulation as a promising new tool in the management of psychological disorders: A systematic review. , Neurosci Biobehav Rev 119, 242-254.
- 46.Salehpour F, Gholipour-Khalili S, Farajdokht F, Kamari F, Walski T. (2020) Therapeutic potential of intranasal photobiomodulation therapy for neurological and neuropsychiatric disorders: a narrative review. , Rev Neurosci 31(3), 269-286.
- 47.Yang M, Yang Z, Wang P, Sun Z. (2021) Current application and future directions of photo biomodulation in central nervous diseases. Neural Regen Res. 16(6), 1177-1185.
- 48.Li X, Liu C, Wang R. (2020) Light modulation of brain and development of relevant equipment. 1, 29-41.
- 49.Zhang D, Shen Q, Wu X, Xing D. (2021) Photobiomodulation therapy ameliorates glutamatergic dysfunction in mice with chronic unpredictable mild stress-induced depression. Oxid Med Cell Longev. 6678276.
- 50.Gujral S, Aizenstein H, Reynolds CF 3rd, Butters M A, Erickson K I. (2017) Exercise effects on depression: Possible neural mechanisms. , Gen Hosp Psychiatry 49, 2-10.
- 51.Urquhart E L, Wanniarachchi H, Wang X, Gonzalez-Lima F, Alexandrakis G. (2020) Transcranial photobiomodulation-induced changes in human brain functional connectivity and network metrics mapped by whole-head functional near-infrared spectroscopy in vivo. , Biomed Opt Express 11(10), 5783-5799.
- 52.Ramezani F, Neshasteh-Riz A, Ghadaksaz A, Fazeli S M, Janzadeh A. (2021) Mechanistic aspects of photobiomodulation therapy in the nervous system. Lasers in Med Sci.pp.1-8.
- 53.Hare B D, Duman R S. (2020) Prefrontal cortex circuits in depression and anxiety: contribution of discrete neuronal populations and target regions. , Mol Psychiatry 25(11), 2742-2758.
- 54.Pinto A P, Guimarães C L, GADS Souza, Leonardo P S, MFD Neves. (2019) Sensory-motor and cardiorespiratory sensory rehabilitation associated with transcranial photobiomodulation in patients with central nervous system injury: trial protocol for a single-center, randomized, double-blind, and controlled clinical trial. , Medicine (Baltimore) 98(25), 15851.
- 55.Yuan Y, Cassano P, Pias M, Fang Q. (2020) Transcranial photobiomodulation with near-infrared light from childhood to elderliness: simulation of dosimetry. , Neurophotonics 7(1), 015009.
- 56.Ribeiro O, Teixeira L, Araújo L, Rodríguez-Blázquez C, Calderón-Larrañaga A. (2020) Anxiety, depression and quality of life in older adults: trajectories of influence across age. , Int J Environ Res Public Health 17(23), 9039.
- 57.Almeida O P, Ford A H, Hankey G J, Golledge J, Yeap B B. (2019) Depression, antidepressants and the risk of cardiovascular events and death in older men. Maturitas.;128: 4-9.
- 58.Tsai S R, Hamblin M R. (2017) Biological effects and medical applications of infrared radiation. , J Photochem Photobiol B 170, 197-207.
- 59.Zein R, Selting W, Hamblin M R. (2018) Review of light parameters and photobiomodulation efficacy: dive into complexity. , J Biomed Opt 23(12), 1-17.
