Abstract
Edentulism is considered a poor health outcome and may compromise quality of life. Implant-supported overdentures provide a good opportunity for dentists to improve the quality of life and oral health. Atrophic mandible poses a significant challenge to successful oral rehabilitation with dental implants. The aim of this case report is to demonstrate the concept of immediate functional loading in the mandible using unsplinted implants to support a locator attachment supported overdenture.
Author Contributions
Academic Editor: Walid AlJallad, United States
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2021 Abdulgani Azzaldeen, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Implant-supported and -retained overdentures have become a widespread and predictable treatment option for edentulous mandibles. Comparatively low costs and simple treatment compared with fixed structures, easiness of hygiene and sometimes also better esthetic results when lost hard and soft tissues need to be replaced are factors that account for the success. 1 A sufficient amount of bone is usually available in the interforaminal area of the mandible to enable im plantation. The number of implants needed for a mandibular overdenture is smaller than for a fixed implant bridge–usually two to four implants–and this is advantageous when the amount of jawbone is reduced. 2 Numerous studies confirm good treatmentresults with two mandibular implants also in the long term. 3 It is generally stated that for an edentulous mandible, two implant overdenture treatment should be the standard of care relative to conventional denture treatment .1, 2, 3, 4
Implant-retained overdentures are widely applied for the rehabilitation of edentulous jaws as it increases retention, stability, enhance masticatory function and reduce alveolar bone resorption by regulating neuromuscular adaptation.5An implant retained overdenture is an alternative form of treatment to the fixed‐implant prosthesis & offers patient an economic alternative.5It has been successfully used to rehabilitate edentulous patients for over 30 years.1, 2The McGill University (Canada) consensus statement on overdentures, issued in 2002, recommended “mandibular 2-implant over dentures” as the first choice standard of care for the edentulous patients.4Overdentures may be retained by bars, balls, magnets, Locator attachment or Ceka attachments.3, 5Compared to other attachments, Locator attachments add versatility to its design. 1, 2, 3, 4, 5
Implant supported overdenture has many advantage over conventional complete denture. It includes minimum anterior bone loss, improved stability by reduces or eliminates prosthetic movement, improved occlusion, increased occlusal efficiency improved chewing efficiency and force, improved retention, improved speech, reduced prosthesis size by elimination palate and denture flange, decrease in soft tissue abrasions and improved patient’s psychological outlook and quality of life.6 When an implant-retained overdenture is advised, The following factors should be considered: 1 cost effectiveness, 2 amount of retention needed, 7 pain cause on the soft tissue, 8 amount of bone available, 5 oral hygiene, 6 patient's social economic status, 9 expectations of the patient, 8 maxillomandibular relationship, 9 status of the antagonistic jaw, and 10 inter-implant distance.9
The aim of this case report is to demonstrate the concept of immediate functional loading in the mandible using unsplinted implants to support a locator attachment supported overdenture.
Case Report
A 63 year old male patient came to our Aesthetics Dental Clinic ,Athens, Greece with the chief complaint of loose fitting lower denture with difficulty in mastication and speech. On examination, patient had resorbed alveolar ridge which lead to inadequate retention of the lower denture prosthesis and patient is known to be a previous denture wearer for past 1 year. The Orthopantomograph findings showed the presence of sufficient bone height and width (Figure 1), with dense cortical bone surrounded by dense trabecular bone. Thus implant supported overdenture was planned with two implants along with independent ball type attachments.
Blood investigations and informed consent was taken after discussing the treatment procedure with the patient and the bystander. Irreversible hydrocolloid impression was made and pre-surgical diagnostic casts were prepared. Inter-occlusal distance was measured in the diagnostic casts. The implant location was marked at B and D positions independent of each other. (Figure 2)
Figure 1.First Visit Pre-operative radiograph
Figure 2.Prpre-operative view of anterior mandibular knife edge ridge.
Surgical Phase
Under antibiotic prophylaxis and standard aseptic protocol, preparation of the patient was done by anaesthetizing the mandibular anterior segment with inferior alveolar nerve block using local anaesthesia of 2% lignocaine with 1:80,000 adrenaline. After the region was anaesthetized, full thickness crestal incision was made with surgical blade number 15 extending from first premolar on right side to first premolar on left side. The mucoperiosteal flap was elevated and bone was exposed. A pilot drill was introduced into the bone and two osteotomy sites were created using piezosurgery device without causing any damage to the adjacent anatomical structures. Two surgical implants (3.5x 11 mm) were inserted (Figure 3) using motor driver at 35 rpm and the landmark of reach was checked with profile gauge. After the implant seating tip has reached the adequate depth, cover screws are placed. Later flaps are approximated, suturing done using 3-0 vicryl suture material. Patient was prescribed with antibiotics and anti –inflammatory coverage. (Figure 4) Patient was recalled on the 7th day of surgery, suture removal was done.
Figure 3.Paralleling pins in each pilot osteotomy indicating their position
Figure 4.A 3.5mm x 11.0mm HA coated implant being inserted into the osteotomy in the area of the mandibular left canine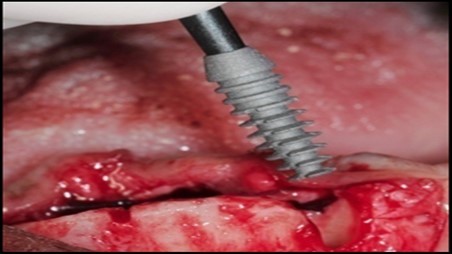
Post operatively after 3 months, osseointegration was evaluated clinically and radiographically (Figure 5a,b) and the implants were well prepared to receive the prosthesis. The second stage surgery was performed in which cover screws were removed and healing abutment were inserted into the implants (Figure 6). After a time period of two weeks, peri-implant soft tissue healing was examined, and existing denture was relined after relieving at the abutment site. Later, the healing abutment is removed using a 1.25 mm hex driver. Internal portion of the implant is irrigated and dried to make sure if it is free of debris and soft tissue. A periodontal probe was used to measure the gingival cuff height at the right and left canine site of implant location. Selected ball abutment were placed onto each implant using 1.25 mm hex driver and 30 Ncm torque wrench (Figure 7A).
Figure 5.a,b. Post-insertion radiographics in the mandibular area right,left,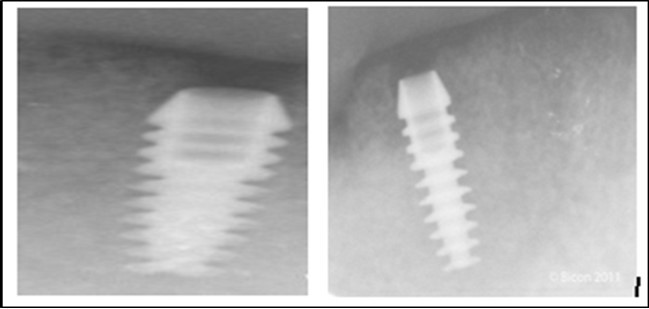
Figure 6.Panoramic radiograph after the insertion of two implants
Figure 7.(A) View of 2.0mm and 5.0mm post Locator Abutments with a 2.0mm post. (B) Placement of the Locator Abutment after the well of implant has been cleaned with alcohol on a cotton-tipped applicator.
A transferable mark with an indelible pencil is placed on top of each ball abutment and old denture is seated to ideally determine the location for attachment housings. It is followed by preparation of recesses in the intaglio surface of the denture to accommodate the housings (Figure 7B). Lingual vent holes are made for escape of excess acrylic. Placement of nylon processing insert into each of the housings is done with insert seating tool. Figure 8 Seating of the attachment housing onto each ball type abutment is done (Figure 9). Undercuts are blocked out under the housing and soft tissue to prevent acrylic resin from locking the denture onto the abutment. Application of self curing acrylic is done into recessed area and around titanium housings for bonding of the housings to denture. Insertion of denture was done and guiding the patient into proper occlusion with the opposing arch. After the curing of acrylic, denture is removed. Excess acrylic is removed around the housings and lingual vent hole later it is polished (Figure 10). Replace nylon retention insert instead of processing insert into the housings. The insert must seat securely in place and be in level with the housings rim. Overdenture is seated over the ball abutments (Figure 11). Proper instructions have been given to the patient on insertion and removal of prosthesis (Figure 12). The patient was recalled at 1 week, 3 weeks, 3 months, 6 months follow up appointments.
Figure 8.View of two Locator Abutments with their metal housing caps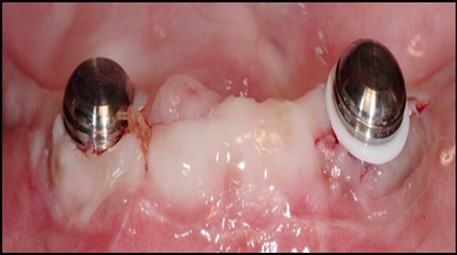
Figure 9.Denture being inserted
Figure 10.Patient applying occlusal force while metal housing caps are being secured into the denture
Figure 11.View of denture after being cleaned and polished
Discussion
The presurgical evaluation of an overdenture patient has the following goals
a. To avoid interference between the prospective positions of the implants, the attachments, and the denture base.
b. To optimize placement of the implants in relation to bone mass and anatomical structures
c. To distribute the implants so that the attachment devices are reasonably arranged
Mandibular denture often presents problem to the patient as well as dental practitioner.11 Mandibular complete overdenture treatment has been available for decades, however its use was limited when the treatment depends on retained teeth or root stumps as overdenture abutments.12, 13, 14, 15 Complete edentulous patients may be presented with option sfor implant supported prosthetic reconstruction that include
1. Full arch implant supported fixed prosthesis, Implant supported overdentures.14, 15 (Figure 12)
2. Surgical treatment is well established for implant placement in the parasymphyseal region of the edentulous mandible. 16, 17, 18, 19 (Figure 8)
Overdenture with pivoting locator attachment allow a resilient connection for the overdenture without any retention loss.6, 7, 8, 9, 10
Many factors contribute to promote the use of individual implants such as: lower costs, improved access for hygiene and cases with small interarch space 14, 15, 20. Thus, an individual approach, i.e., individual dental implants treatment is more efficient, resulting in the lowest cost and more effective for most edentulous patients 20
According to the literature, it appears that “interarch space required for the retention of a prosthesis to the implant (distance from the shoulder of the implant to the incisal edge) is about 12 to 14 mm as follows: a thickness of 2–3 mm of soft tissue is generally present above the implant, an area of 2 mm from the lining of the edentulous ridge to the bar needs to be present for suitable cleaning 15, 4.5 mm bar thickness, 2 mm for the acrylic resin and the rider 21 and 3 mm for the teeth” 22. Most attachment systems with staples include height of the matrix and the abutment, ranging between 5–6 mm 23. (Figure 7A,B,) In conclusion, patients with well-preserved ridge, who have lost teeth due to caries benefit from reduced interarch space for an implant overdenture. In addition to this, the space often limited interferes with the reinforcement of the prosthesis making it hard for the dentist to use the space required for devices such as staple systems 23. “Thinning the soft tissue during the surgical act and the use of internal connection to implants can help us overcome the problem of limited vertical space” 22.
For atrophic mandibular ridge, implant supported overdentures proves to be the most efficient of all. Considering the financial resources of the patient and also the presence of inferior quality of bone in posterior region compared to anterior of the same arch creates the need for the placement of two implants with ball attachments in the anterior region of mandibular arch which is located anterior to foramens.6, 8, 9, 10, 24
The use of two implants has shown to be biomechanically sound which provided better prosthetic stability and prevented rotational forces of the components.6, 8, 14, 15By placement of two independent implants at the same height, equidistant from the midline and parallel to each other with proper angulation prevents wearing away or disengagement of the attachments.25 Additionally, the posterior region of the overdenture rocks downward resulting in soft tissue loading over buccal shelves for support also with hinge rotation being 90 degree to the rotation path avoids various complications such as abutment screw loosening, crestal bone loss and implant failure.26, 27, 28Though nowadays, single piece implants have become popular due to its innumerable benefits, correct angulation is the most catastrophic mistake thereby achieving parallelism becomes crucial.27, 28
So in this case conventional two piece implants were chosen over the single piece implants. Relatively, success rate of two implants is equivalent to that of the overdenture supported by four or six implants hence replacement of edentulous mandibular ridge with two implants in the anterior seems to be a logical treatment solution. 14, 15, 24, 25, 26, 27, 28
General criteria for survival and success of implants have been used to evaluate the efficacy of immediately loading mandibular implants. For example, survival criteria include how the implant performs, particularly regarding the absence of pain, infection, and paresthesia. Implant immobility and the absence of periimplant radiolucency under radiography are 2 more criteria of implant survivability.6, 7 Success criteria include the additional element of absence of vertical bone loss; specifically, less than 1 mm during the first year and less than 0.2 mm annually thereafter. Granted that success rates for immediatel oading of implants in the edentulous mandible are not as high as rates for the traditional 2-stage approach, conditions nevertheless often warrant the 1-stage surgical option described here.7, 8, 9 (Figure 12).
Clinician caution regarding hard tissue and soft tissue concerns in the anterior mandible is warranted whenever a 1-stage protocol is attempted; however, immediate or delayed loading of implants in a 1-stage protocol presents the clinician and patient with numerous benefits.10, 16, 18
Complications seen with implant overdentures are generally biological and technical or mechanical and more mucosal hyperplasia has been noticed with bars than with ball attachments.7 It has been supposed that an insufficient space beneath the bar–which prevents proper cleaning– may cause a soft-tissue inflammatory response under the bar attachment.8, 9 Another reason for mucosal hyperplasia with bars could be the less precise settling of the denture base to the mucosa compared with ball overdentures.10, 16Periimplant mucositis is rather often seen around implants. The incidence (an average of 19 %) associated with implant overdentures is greater than with fixed implants.9 The most common technical complications with implant overdentures are loosening of the retentive mechanism, usually seen in about 30 % of cases.6, 7 In addition, fracture of the retentive anchor, occlusal screw loosening with bars, fracture of the acrylic base material or broken teeth and fractured bars are common findings. Resilient attachments were observed to more frequently have broken, loose, or lost female parts and a need for repairs and relining of the denture base, whereas rigid bar attachments more typical need tightening of the bar retainers.10, 16 It has been shown that attachments wear over time and lose their retention force. A rigid milled bar attachment on four-implant overdentures has been shown to cause less prosthetic maintenance compared with resilient denture attachments with ovoid bars.7, 8, 9
In our case, we chose this kind of treatment because of insufficient restorative space available, which was less than 9 mm. At the same time, we considered the fact that in time it is possible to lose an implant or two, a condition that can be remedied without much need of the laboratory help with refurbishing the denture, accordingly to McGill’s consensus. Also, there were financial agreements with the patient that lead to this treatment plan. Among other factors that guide the selection of attachment devices, we include their height, which significantly contribute to reducing the potential of fracture of the denture base in the case of insufficient acrylate thickness. The advantage of using the Locator attachment system is that when a gasket replacement is needed it is not mandatory to remediate the entire device within the denture base.
Using 2 implants and retentive anchors for the retention of a mandibular complete denture is, in terms of immediate costs, one of the most affordable implant procedures. 8, 9, 14 With ideal placement of the implant, the stability of the prosthesis is excellent and the lingual dimensions of the denture can in some cases be reduced to the level of mylohyoid line, providing more space for the tongue and greater comfort than with conventional complete dentures.8, 9, 10, 15 However, if the labial musculature is tense or the amount of attached gingiva is limited, the implants should not be placed too deep or too labially, which might prevent gingival growth over the abutments. In those cases, ball anchor abutments with elevated shoulders can be used to improve implant anatomy.8, 9, 10 (Figure 12).
Conclusions
In conclusion, within the limits of this interim report, immediate loading of two-implants supporting a locator retained mandibular overdenture seems to be a suitable treatment option. The marginal bone level changes around immediately loaded implants are comparable to those seen around implants loaded with a torque do not effect peri-implant bone loss. Implant survival of immediately loaded implants may be lower than those loaded with a delayed protocol, but this needs to be confirmed in future investigations with a larger sample size. Elayed protocol, at 6 months postsurgery. Implant length and peak insertion.
References
- 1.Zarb G A, Schmitt A. (1990) The longitudinal clinical effectiveness of osseointegrated implants: the Toronto Study. Part II: The prosthetic results. J Prosthet Dent. 64(1), 53-61.
- 2.Zarb G A, Schmitt A. (1990) The longitudinal clinical effectiveness of osseointegrated implants: the Toronto Study. Part III: Problems and complications encountered. , J Prosthet Dent 64(2), 185-94.
- 3.Adell R, Eriksson B, Lekholm U, Brånemark P I, Jemt T. (1990) A long-term follow-up of tissue integrated implants in the treatment of the totally edentulous jaw. Int J Oral Maxillofac Implants. 5(4), 347-59.
- 4.Mericske-Stern R, Steinlin Schaffner T, Marti P, Geering A H. (1994) Peri-implants mucosal aspects of ITI implants supporting over dentures. A fiveyear longitudinal study. Clin Oral Implants Res. 5(1), 9-18.
- 5.Atwood D A, Coy W A. (1971) Clinical, cephalometric, and densitometric study of reduction of residual ridge. , J Prosthet Dent 26, 280-295.
- 6.Abu-Hussein M, Abdulgani A, Bajali M, Chlorokostas G. (2014) The Mandibular Two-Implant Overdenture. , Journal of Dental and Allied Sciences 3(1), 58-62.
- 7.Azzaldeen Abdulgani, Musa Bajali, Nikos Kontoes, Muhamad AbuHussein. (2015) Atrophied Edentulous Mandible with Implant-SupportedOverdenture; A 10year follow-up. , Journal of Dental and Medical Sciences 14(12), 114121.
- 8.Muhamad Abu-Hussein, Chlorokostas G, Abdulgani A. (2017) Ιmplant-Supported Overdentures: Clinical Review. 6(2), 403-411.
- 9.Abdulgani Azzaldeen, Nezar W, Muhamad A. (2016) Implant-supported restorations in the anterior region. , IOSR Journal of Dental and Medical Sciences
- 10.George Chlorokostas, Muhamad A, Abdulgani A. (2016) Immediate Loading With Mini Dental Implants In The Fully Edentulous Mandible. , Journal Of Dental And Medical Sciences
- 11.Tallgren A. (1972) The continuing reduction of the residual alveolar ridges in complete denture wearers: a mixedlongitudinal study covering 25 years. , J Prosthet Dent 27, 120-132.
- 12.Tallgren A. (1966) The reduction in face height of edentulous and partially edentulous subjects during long-term denture wear: a longitudinal roentgen graphic cephalometric study. , Acta Odontol Scand 24, 195-239.
- 13.Misch C E. (2008) The Edentulous Mandible: An Organized Approach to Implant-Supported Overdentures. Contemporary Implant Dentistry. 3rd ed. St. Louis 293-313.
- 14.Abu-Hussein M, Georges C, Watted N, Azzaldeen A. (2016) A Clinical Study Resonance Frequency Analysis of Stability during the Healing Period. , Int J Oral Craniofac Sci 2(1), 065-071.
- 15.Abu-Hussein M, Watted N, Shamir D. (2016) A Retrospective Study of the AL Technology Implant System used for Single-Tooth Replacement. , Int J Oral Craniofac Sci 2(1), 039-046.
- 16.Abu-Hussein M, Abdulgani A. (2014) Mandibular implant overdenture retained with o-ring ball. , Int J Dent Health Sci 1(6), 984-991.
- 17.Mai A, Azzaldeen A, Nezar W, Chlorokostas G, Muhamad A H. (2016) Extraction and Immediate Implant Placement with Single-StageSurgical Procedure: Technical Notes and a Case Report. , J Dent Med Sci 15, 95-101.
- 18.Mai Abdulgani. (2016) Abdulgani Azzaldeen, Watted Nezar, Chlorokostas Georges, Abu-Hussein Muhamad. Extraction and Immediate Implant Placement with Single-Stage Surgical Procedure: Technical Notes and a Case ReportJournal of Dental and Medical Sciences 15(11), 95-101.
- 19.Abu-Hussein M, Azzaldeen A, Aspasia S A, Nikos K. (2013) Implants into fresh extraction site: A literature review, case immediate placement report. , J Dent Implant 3, 160-164.
- 20.Vogel R C. (2008) Implant overdentures: a new standard of care for edentulous patients current concepts and technique, Compend Contin Educ Dent. 29(5), 270-276.
- 21.Morris J C, Khan Z, von Fraunhofer JA. (1985) Palatal shape and the flexural strength of maxillary denture bases, J Prosthet Dent. 53(5), 670-673.
- 22.Phillips K, Wong K M. (2001) Space requirements for implant-retained bar-and-clip overdentures, Compend Contin Educ Dent. 22(6), 516-518.
- 23.Pasciuta M, Grossmann Y, Finger I M. (2005) A prosthetic solution to restoring the edentulous mandible with limited interarch space using an implant-tissue-supported overdenture: a clinical report, J Prosthet Dent. 93(2), 116-120.
- 25.Kline K W, Misch C.Elastometric O-ring implant design principles. Dental Implant Prosthetics. Partial and complete Edentulous Maxilla Implant Treatment Plans. Capítulo.;15
- 26.Burns D R, Unger J W, Elswick R K, Beck D A. (1995) Prospective clinical evaluation of mandibular implant overdentures: Part I—Retention, stability, and tissue response. , The Journal of prosthetic 73(4), 354-63.
Cited by (1)
- 1.Chaudhry Ammara, Shakeel Sadia, Shahid Tayyaba Nayab, Anwar Malik Adeel, Tariq Khaloud, et al, 2025, Knowledge, Attitudes, and Practices towards Early Childhood Caries among Affluent Parents of Lahore, Pakistan Journal of Health Sciences, (), 30, 10.54393/pjhs.v6i2.2552

