Author Contributions
Academic Editor: Kunwarjeet Singh, Associate Professor, Department of Prosthodontics, Dental materials and implantology, institute of dental studies and technologies
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2015 Cimara Fortes Ferreira
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Abstract
In order to achieve functional and esthetic oral rehabilitations, dental implants must be placed at an ideal tridimensional position in the alveolar bone. A clinical case is presented of a 49-year-old female with a severely resorbed pre-maxilla. Bone augmentation was conducted using the “tent pole” technique with human recombinant morphogenetic bone protein-2 embedded in an absorbable collagen sponge and deproteinized bovine bone. In addition, a titanium mesh was adapted over the graft to provide support. At 8 months post-op, a cone beam computerized tomography (CBCT) scan showed significant bone consolidation. An ideal pre-maxilla ridge with more than 14 mm of vertical and 10 mm of horizontal width was observed. Four dental implants were placed. Re-entry was 6 months later. Individual crowns were made to substitute the incisors, which were in function for the 1-year follow-up.
Introduction
The use of dental implants for oral rehabilitations has become a routine procedure in the practice in dentistry. An increasing number of fully and partially edentulous patients seek this type of rehabilitation for the advantage of being a fixed and conservative solution to the tooth loses. Dental implants must be planned and placed at the best tridimensional position in the alveolar process in order to restore masticatory and phonetic functions, in addition to esthetics. For this purpose, the treatment plan is governed primarily by the prosthetic design.1 A significant number of patients present with bone defects that do not allow a prosthetically driven implant placement due to lack of bone resulting from numerous etiologies, such as: periodontal disease, traumatic dental extraction and/or physiologic absorption.2
Autogenous bone grafts are considered the gold standard of augmentation materials for the treatment of oral and maxillofacial bony defects.3 The autogenous grafts shows advantages over the other graft types due to their ostegenic, osteoinductive and osteoconductive characteristics. This graft can be harvested from mandible, maxilla, tibia, cranial vault and iliac crest.
However, the autogenous bone grafts require the need of a second surgical site, which increases postoperative morbidity, pain, sensibility alterations, scars and infections especially at the donor site. In addition, it incurs additional costs.4 To overcome these disadvantages, researches have strived to develop alternative materials to substitute the autogenous bone grafts.
The human recombinant morphogenetic bone protein 2 (rhBMP-2) is a growth factor associated with the proliferation of mesenchymal cells and their differentiation into osteoblasts.5 rhBMP-2 is the most researched and published bone growth factor and has shown to be of great importance in the success of bone reconstruction procedures. The use of rhBMP-2 has been used for augmentation of: clefts6, experimental critical-size defects7, continuityor mandibular alveolar bone defects3 and sinuses.8 All these studies have shown biologically the role of rhBPM-2 on bone formation and pointed out that its clinical use can be an alternative to autogenous bone graft in some clinical situations.
Few studies have used rhBMP-2 for rehabilitation of the atrophic pre-maxilla. The objective of this case study is to present an alternative technique to autogenous bone graft to reconstruct a severely absorbed pre-maxilla using rhBMP-2 associated with lyophilized bone graft and titanium mesh.
Case Report
A 49-year-old female presenting a severely resorbed pre-maxillary as a result of previous autogenous bone graft presented to the clinic. Treatment plan was conducted by means of the fabrication of a prototype anatomic model by means of a CBCT scan (Figure 1). A titanium mesh was fabricated on this model to shape an ideal ridge, with normal height and width. Four dental implants were planned to substitute teeth number 7, 8, 9 & 10 for single unit crowns.
Figure 1.CBCT showing presence a significant bone defect of the pre-maxilla.
The surgical procedure was done under intravenous sedation using Fentanyl and Versed. Local anesthetic was used and a supra-crestal horizontal incision made on the palatal aspect of the anterior maxilla. A mucoperiosteal flaps were elevated, exposing a severely resorbed ridge of the pre-maxilla (Figure 2). Decortication was conducted with a round carbide bur in order to perforated the cortical aspect of the bone and expose the cancellous bone, to increase vascularity to the recipient site. Three screws were fixed parallel to the adjacent teeth, serving as “tent pole”. The screws had 14 mm length and approximately 6-8 mm of the tenting screws were exposed to the oral cavity (Figure 3). An absorbable collagen sponge (ACS) carrier/matrix was embedded with 12 mg of rhBMP-2 at 1.5 mg/mL (Infuse® Medtronic Sofamor Danek, Memphis, TN, USA) and allowed to absorb for approximately 20 min. The rhBMP-2/ACS was cut into strips, half of the strips were added to the natural bone mineral component derived from bovine bone (Geistlich Bio-Oss® granules small - 0.25 to 1 mm, Geistlich Pharma, Germany). Initially, some strips of rhBMP-2/ACS were placed over the buccal aspect of the residual alveolar ridge of the pre-maxilla, followed by strips mixed with bovine bone (Figure 4). The three screws were fully covered by rhBMP-2/ACS strips. Finally, a titanium mesh was adapted over the entire rhBMP-2/ACS graft and fixed with 2 monocortical screws, one on the buccal aspect and one on the palatal aspect of the ridge, respecting a 2 mm distance from the mesh to the adjacent teeth (Figure 5). Extensive undermining incision was conducted on the apical aspect of the buccal flap in order to achieve primary closure.
Figure 2.Occlusal view of the pre-maxilla after elevation of amucoperiosteal flap. Noteright and left pre-maxilla buccal plate concavities due to severely resorbed ridge. The central tenting screw is located mid-way into the nasal spine.
Figure 3.Frontal view of the pre-maxilla after elevation of amucoperiosteal flap. Note 6-8 mm of the tenting screws length are exposed.
Figure 4.Occlusal view of the pre-maxilla after placement of strips of the rhBMP-2/ACS added to the natural bone mineral component derived from bovine bone.
Figure 5.Perspective view of the pre-maxilla showing a titanium mesh adapted over the entire rhBMP-2/ACS graft and fixed with 2monocortical screws, one on thebuccalaspect and oneon the palatal aspect of the ridge, respecting a 2 mm distance form the mesh to the adjacent teeth
At the 8-months follow-up, a CBCT scan showed consolidation of the grafted material with the recipient bone (Figure 6). A second surgical procedure was conducted under local anesthesia and oral sedation in order to remove the titanium mesh. At this appointment, the pre-maxilla showed to be significantly augmented (Figure 7) with the dimension of 14 mm in height and 10 mm in width. The bone characteristics were soft, erythematous, with a cancellous texture. Four dental implants (Biomet 3I certain®, USA) were inserted, with no more than 25 Ncm2 of primary stability (Figure 8). The implants were uncovered 6 months later for initiation of the prosthetic rehabilitation using 4 single-unit crowns. One-year follow-up showed to be uneventful (Figure 9).
Figure 6.CBCT scan 8 months post ridge augmentation. Note significant increase in bone augmentation of the pre-maxilla. Presence of implants for sites #2, 3, 4, 11, 12 and 13 after right and left sinus lifts were performed.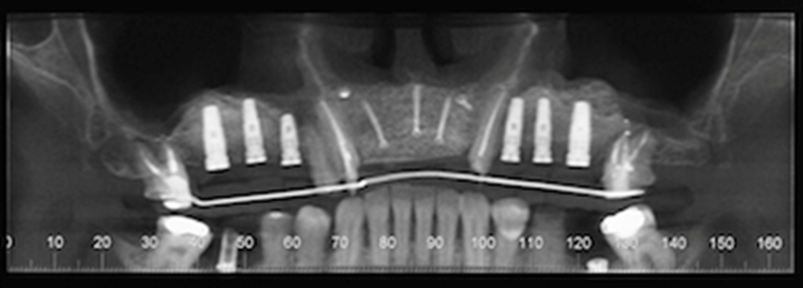
Figure 7.Re-entry at 8-monthspost-op shows a clinically significantly augmented maxilla. Occlusal viewshows implants (Biomet 3I certain®, USA) # 7 and 10 placed.
Figure 8.Perspective view of the augmented pre-maxilla with implants(Biomet 3I certain®, USA) #7, 9, 10placed. and #8 beingplaced.
Figure 9.One-year follow-up after delivery of 4 porcelain-fused-to-metal crowns.
Discussion
Different surgical techniques have been employed to treat the severely atrophic pre-maxilla. Autogenous bone grafts to augment the atrophic maxilla following the insertion of dental implants have become the treatment of choice for maxillary and mandibular reconstructions. However, autogenous bone grafts present disadvantages, such as: sensory disturbances, wound dehiscence, infections in the grafted area and morbidity of the donor site.These disadvantages are more evident whenever extra-oral sites, such as: iliac crest, tibial bone or cranial vault are used.4 The present case report shows a severe bone atrophy that would require an extra-oral donor site, if autogenous bone graft had been chosen. While evaluating the possible complications and unpredictability involved with using an extra-oral graft, this treatment option was rejected.
Vertical distraction osteogenesis could have been a treatment option for this case to restore the lost vertical bone height. However, this technique is indicated when there is at least 10 mm of bone height and in this case, the residual pre-maxilla ridge had less than 8mm, contraindicating this procedure. Furthermore, alveolar osteogenic distraction in the anterior maxilla is unpredictable for cases that need more than 10mm.9
Short implants appears to be an attractive treatment option due to the simple surgical procedure, with limited morbidity, avoidance of bone grafts and high survival rates.5 However, this treatment option is not indicated for esthetic areas, especially in this case where the patient presented a gummy smile, which would compromise the esthetics.
BMPs are members of the transforming growth factor-β superfamily of growth factors. Twenty unique BMP ligands have been identified and categorized into subclasses based on amino acid sequence similarity. Urist, in 1971, was the first to report that the BMPs played an important role into the modulation and differentiation of mesenquimal cells into osteoblasts.10, 11 In 1988, Wozney synthesized a BMP-2 through recombination, cloning and isolation from genes originally obtained from a purified bovine bone extract.12The only BMP currently available for grafting of maxillofacial implant sites is rhBMP-2, which is commercialized in a powder that must be reconstituted with a diluent and then applied to the ACS. The FDA in the United States and the ANVISA in Brazil allowed the clinical use of rhBMP-2 for sinus lift and localized alveolar ridge defects associated with extraction socket, reconstruction of large alveolar bone defects, and cleft palate. In the present clinical case, a modified approach to reconstruct a severely atrophic pre-maxilla was used. This case demonstrated the high potential of rhBMP-2 for bone reconstruction.
ACS is 90% air, which is an inadequate scaffold in larger-volume defects.13 In large defect reconstructions, especially for vertical augmentation, a scaffold is necessary for bone formation. Because of these requirements, a natural bone mineral component derived from bovine bone and a titanium mesh were used. The proposed technique proved to be a successful due to the scaffold serving for bone formation which extended beyond the limitations of the titanium mesh. In addition, the natural bone mineral component derived from bovine bone was used to promote a higher bone density due to its higher osteocondutive potential.
The reconstructive technique presented showed to be successful in the augmentation of severely atrophic pre-maxilla for the rehabilitation with dental implants. Further studies are necessary to verify if the success obtained in this clinical case is statistical significance.
References
- 1.Wikesjo U M, Sorensen R G, Wozney J M.Augmentation of alveolar bone and dental implant osseointegration: clinical implications of studies with rhBMP-2. The Journal of bone and joint surgery American volume 2001;83-A Suppl1:. 136-145.
- 2.Wikesjo U M, Polimeni G, Qahash M. (2005) Tissue engineering with recombinant human bone morphogenetic protein-2 for alveolar augmentation and oral implant osseointegration: experimental observations and clinical perspectives. Clin Implant Dent Relat Res. 7, 112-119.
- 3.Herford A S, Stoffella E, Tandon R.Reconstruction of mandibular defects using bone morphogenic protein: can growth factors replace the need for autologous bone grafts? A systematic review of the literature. Plastic surgery international 2011;2011:. 165824.
- 4.Rawashdeh M A, Telfah H. (2008) Secondary alveolar bone grafting: the dilemma of donor site selection and morbidity. The British journal of oral & maxillofacial surgery. 46, 665-670.
- 5.Annibali S, Cristalli M P, Dell’Aquila D, Bignozzi I, La Monaca G et al. (2012) Short dental implants: a systematic review. , Journal of dental research 91, 25-32.
- 6.Mostafa N Z, Talwar R, Shahin M, Unsworth L D, Major P W et al. (2015) Cleft palate reconstruction using collagen and nanofiber scaffold incorporating bone morphogenetic protein in rats. Tissue engineering Part A. 21, 85-95.
- 7.Park J, Ries J, Gelse K. (2003) Bone regeneration in critical size defects by cell-mediated BMP-2 gene transfer: a comparison of adenoviral vectors and liposomes. Gene therapy. 10, 1089-1098.
- 8.Jensen O T, Kuhlke K L, Leopardi A, Adams M W, Ringeman J L. (2014) BMP-2/ACS/allograft for combined maxillary alveolar split/sinus floor grafting with and without simultaneous dental implant placement: report of 21 implants placed into 7 alveolar split sites followed for up to 3 years. Int J Oral Maxillofac Implants;29: e81 - 94.
- 9.Ettl T, Gerlach T, Schusselbauer T, Gosau M, Reichert T E et al.Bone resorption and complications in alveolar distraction osteogenesis. Clinical oral investigations 2010;14:. 481-489.
- 10.Urist M R, Strates B S. (1971) Bone morphogenetic protein. , Journal of dental research 50, 1392-1406.
Cited by (2)
- 1.Boroojeni Helia Sadat Haeri, Gharehdaghi Niusha, Moghaddasi Sahar, Khojasteh Arash, 2023, , , (), 143, 10.1007/978-981-19-8602-4_9
- 2.Alraei Kamel, Shrqawi Jameel, Alarusi Khawlah, Shibli Jamil Awad, 2021, Application of Recombinant Human BMP-2 with Bone Marrow Aspirate Concentrate and Platelet-Rich Fibrin in Titanium Mesh for Vertical Maxillary Defect Reconstruction prior to Implant Placement, Case Reports in Dentistry, 2021(), 1, 10.1155/2021/6691022
