Fragiles but Resilient. The Key Strategies to Cope with Pandemic in Persons with Multiple Sclerosis. A Controlled Web Survey
Abstract
Background
SARS-CoV-2 pandemic represented an unexpected psychological stress, being a major threat to health and limiting daily’s life, especially for the fragile population. How could the people with (pw) Multiple Sclerosis (MS) cope with this emergency?
Objective
To observe the pwMS’s psychological reaction in comparison with non affected persons and to evaluate the impact of lifestyle changes on psychological symptoms, due to the pandemic.
Methods
The study was observational, retrospective, controlled, focused on good clinical practice and conducted at Niguarda Hospital. PwMS and controls filled a web survey containing anamnestic data, habits, depression and anxiety self-questionnaires. The primary outcome was the pwMS’s psychological anxiety and depression score compared with controls.
Results
On April, 10 2020, 88/165 pwMS and 187 controls joined the study. Unexpectedly, no significant differences between groups were observed for depression mean score: 6.6(5.2) in pwMS and 6.2(4.8) in controls and for anxiety: 5.9(4.8) and 5.0(4.2). PwMS focused on health concern more often than controls, but they respected the restrictions more easily and benefited from practical activities more than controls.
Conclusion
PwMS showed a proper psychological resilience in comparison with controls. These findings might guide the clinical interviews and suggest both the areas to be supported and the strengths to be promoted in pwMS.
Author Contributions
Academic Editor: Christopher Gardner-Thorpe, Diploma in the History of Medicine of the Society of Apothecaries (DHMSA), London
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2022 Annalisa Sgoifo, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Multiple Sclerosis (MS) is a chronic, autoimmune, inflammatory and neurodegenerative disease that predominantly affects young individuals, between the ages of 20 and 50, mostly female 1. People with MS (pwMS) present a high burden of neuropsychiatric comorbidities, such as anxiety and depression (A/D) 2, also associated with fatigue, physical symptoms and cognitive disability, resulting in a lower quality of life and decreased compliance. These conditions are associated with psychological stress and could be responsible of the disease exacerbation 3.
On February 21st, 2020 the first cases of SARS-CoV-2 infection were diagnosed in Italy and on March 11th, eighteen days after, the World Health Organization declared that the infection had become pandemic. Pandemic represents a sudden and major threat to health, that is an unexpected psychological stress, worsened by the general “lockdown” (the necessary severe restrictions on daily life were decided from March 10th, to May 3rd). The phantom of viral infection, the sudden psychosocial changes, the announced economic consequences and the confusing and alarmist information led people to fear and fear can increases anxiety and mental distress, also worsening psychiatric symptoms 4. People with autoimmune and inflammatory diseases, or treated with immunosuppressive therapy, were immediately considered at a major risk of harmful infection 5. As a precaution, researchers and clinicians payed a great attention to these groups of patients.
Obviously, pwMS are part of the fragile population but, from a psychological point of view, this means that they are paradoxically more used to manage a chronic but unpredictable condition compared to healthy people. Especially in the initial stages of the diagnostic and therapeutic path for MS, and then for relapses, they suffer a forced suspension of their routine habits and professional life (due to the symptoms and the medical visits). Similarly, the SARS-CoV-2 pandemic and the restrictions did the same on the general population. In fact, a great and serious impact on mental human health was described as a result of actual and past pandemics, particularly involving vulnerable groups: older adults, the immunocompromised, subjects with previous clinical and psychiatric conditions, but also relatives of infected patients, residents of high-incidence areas, quarantined people and health professionals, going beyond the division between healthy/diseased people 4, 6.
How did this higher risk of infection impact on the psychological status of pwMS during the restrictions? Could the concern for health and for MS, considered as an adjunctive risk factor for SARS-CoV-2 poor prognosis, have stressed the pwMS or have motivated them to better tolerate the lockdown? Moreover, might the pwMS have gained greater resilience to lockdown compared to the general population?
Objectives
We conducted a study to observe the psychological reaction of pwMS during the SARS-CoV-2 emergency. We considered A/D symptoms to find out possible patterns among lifestyle factors and psychological distress. These findings could address the clinical interview and suggest both the critical areas to be supported and the strengths to be promoted. We also collected the same data from volunteers non affected by MS (controls) to compare their answers with those of the fragile MS population.
The primary outcome concerned the rates of anxiety and depression scores in pwMS compared with controls.
The secondary objectives considered the effects of anamnestic and lifestyle factors on A/D. Resilience of pwMS, already studied for adaptation to MS, was also explored in this setting.
Methods
The study design was observational, controlled, based on a web survey, and focused on improvement of quality of the clinical practice. It was approved by the Ethic Committee “Milano Area 3” and conducted at Niguarda Hospital according to the Good Clinical Practice and the Declaration of Helsinki. Personal data have been collected and analyzed in pseudo-anonymous and aggregate form, according to regulation 679/2016 EU.
All subjects were informed on the aim of the study and provided the informed consent. PwMS were enrolled according to the following criteria: adult subjects diagnosed with Multiple Sclerosis 7 who have indicated a valid email address to be contacted by the Niguarda MS Center. Controls were invited to participate using WhatsApp tm viral message in four different towns besides the city of Milano to involve the northern, central and southern regions of Italy and according to the following eligibility criteria: adult subjects not diagnosed with MS and not working as health professionals.
Statistical Analysis
All data have been validated and then submitted to usual descriptive statistics. Binary and nominal categorical variables have been described with relative and absolute frequency tables, while continuous and ordinal variables have been described as mean and standard deviation or median and range, depending on their distribution, checked by the Shapiro-Francia test. Comparison between nominal and binary variables were carried out by the Fisher's exact test, whereas comparisons between continuous variables were done with the Student's t test, the Welch's test, or with the Mann-Whitney U test with exact algorithm, depending on their distribution and on the homogeneity of variances. Comparisons between ordinal variables were always carried out by the exact Mann-Whitney U test.
Correlations between variables were calculated using the Pearson's r, or the Spearman's ρ, again, depending on the distribution.
Materials
On April 10th 2020, a total number of 165 pwMS followed up by the MS Center of the Niguarda hospital in Milan, received by email an invitation to join the study by filling out a web survey. The survey was built using Google Form, a platform by Google LLC. The study collected the answers about lifestyle, habits and psychological status referred to the two weeks from March 27 to April 10.
The web survey provided five sections totally reported in the Supplementary Table 4A the first included the study and the privacy disclosures with the consent. The second section contained multiple choice questions about: socio-demographics, MS anamnestic data and ongoing treatment, previous history of anxiety and depression with related treatment, satisfaction with the information received by the MS Center, changes in MS treatment. The third section referred to the health perception, the need for economic or logistic support and the lifestyle habits during the SARS-CoV-2 restrictions. These last were: the everyday life coping strategies, the home and the family relationships, the physical activities, the job changes, the impact of media news. The fourth section investigated: the feared or objective SARS-CoV-2 symptoms, the mourning of relatives, friends or neighbors caused by the virus. The final section consisted of two structured self administered questionnaires: “The 7-items Generalized Anxiety Disorder Scale” (GAD-7) 8 for anxiety and “The Patient Health Questionnaire” (PHQ-9) 9 for depression. Both of these brief screenings were based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) (DSM-IV-TR) 10, respectively for the General Anxiety Disease and for the Major Depressive Episode. The items had response options ranging from 0 to 3 (0=Not at all; 1=Several days; 2=More than half the days; 3=Nearly every day) with higher scores indicating more severe symptoms.
The GAD-7 has a sum score ranging from 0 to 21. This measure was validated in the general population 9 and in other specific populations, including in MS for clinical and research purposes 12. A cut point of 10 or greater provided sensitivity and specificity higher than 0.80 8 .
The PHQ-9 includes nine items with a sum score ranging from 0 to 27; it’s commonly used for screening and diagnosis of depression also in pwMS 13. A cut-off score greater than or equal to 10 has been suggested as indicative of significant depressive symptoms 14 and it has also been considered a suitable screening tool to measure depression in pwMS.
Results
Demographics
A total number of 88 web surveys were correctly returned from MS outpatients and 187 from controls. Please refer to (Table 1) for sample characteristics and to (Table 2) for MS treatment details and changes due to the pandemic.
Table 1. Socio-demographic and clinical characteristics of participants| Characteristics | pwMS (n.88) | controls (n.177) | p= |
|---|---|---|---|
| Female sex, No. (%) | 64 (73%) | 122 (69%) | p=0.773 * |
| Age, mean (SD), y | 44.5 (9.8) | 43.9 (11.3) | p=0.641 ** |
| Self employed, No. (%) | 7 (8) | 16 (9) | p=0.812 * |
| Employed, No. (%) | 58 (65.9) | 124 (70.1) | |
| Other job condition: | |||
| Fired/suspended for the pandemic | 4 (4.5) | 5 (2.8) | |
| Unemployed, No. (%) | 9 (10.2) | 8 (4.5) | |
| Retired, house wife, student, No. (%) | 10 (11.4) | 24 (13.6) | |
| Smart working, No. (%) | 32 (36.4) | 60 (34.7) | p=0.786 * |
| Satisfying house living space | 70 (80.5) | 144 (84.7) | p=0.384 * |
| Sport, No. (%) | 32 (36.4) | 85 (48) | p=0.046 *** |
| Sport suspended, No. (%) | 19 (21.6) | 44 (24.9) | |
| No physical activity, No. (%) | 37 (42) | 48 (27.1) | |
| SARS-COV2 symptoms (subjective), No. (%) | 13 (14.8) | 46 (26) | p=0.042 * |
| Mourning for SARS-COV2 of known people, No. (%) | 24 (27.3) | 43 (24.3) | p=0.652 * |
| MS treatment details | pwMS(n.88) |
|---|---|
| Median EDSS (range) | 2 (1-7) |
| MS duration, mean (SD), y | 13 (11.5) |
| No MS treatment No. (%) | 10 (11.3) |
| MS treatment to be started, No. (%) | 3 (3.4) |
| MS treatment: | |
| first line - injective, No. (%) | 32 (36.4) |
| first line - oral, No. (%) | 24 (27.3) |
| second line - oral, No. (%) | 10 (11.4) |
| second line - infusion, No. (%) | 9 (10.2) |
| MS treatment delayed | 2 (2.3) |
| MS treatment delivered in the MS center closer to the patient’s home | 3 (3.4) |
PwMS reported satisfaction regarding the communication with the MS Center in 81% of cases. 8/88 pwMS asked for logistic support for food or other activities and in one case no help was given.
The controls answered for the most part from the North of Italy (87.5% of cases). 95% of subjects report a discrete-good healthy state, while a chronic condition was reported in 20% of cases. 3/177 controls asked for logistic support for food or other activities and 4/177 asked for economic aid, but in 2/177 the financial help was not given.
Primary Outcome
Considering the mild cut-off suggested for PHQ-9≥10, the depressive symptoms occurred in 24.5% of pwMS and in 17.6% of controls, with a comparable mean score.
According to the cut-off GAD-7≥10, deriving from the ROC analysis, the 16.4% of the sample presented moderately anxious symptoms; the mean score was overlapping in the two groups and means “mild symptoms”. No significant difference between groups were detected for A/D scores.
Anamnestic Data
Psychological data and treatments were collected in Table 3. As expected, A/D symptoms were more frequent in MS group compared to controls. PwMS reporting to suffer from depression, were confirmed to have a more severe PHQ-9 score (p<0.0001) and those still receiving support with alternative strategies (telemedicine) resulted more depressed compared to the others (p=0.014). Differently, we noted that all the subjects referring to be anxious, presented more severe GAD-7 score (p<0.0001) but the anxiety status of supported persons didn’t differ from that of non supported, maybe because in the latter the concern about the pandemic might have worsened the anxiety status. About MS history, the Spearman Correlation between actual psychological symptoms and time from diagnosis was not significant (GAD-7: n. 87, rho -0.1486, p=0.17; PHQ-9: n. 83, rho -0.1040, p=0.35).
Table 3. Psychological symptoms and treatment| A/D symptoms and treatment | pwMS (n.88) | controls (n.177) | p= |
|---|---|---|---|
| A/D symptoms reported, No. (%) | 23 (26.1) | 21 (11.9) | p=0.005 * |
| No A/D treatment, No. (%) | 65 (73.8) | 148 (83.6) | p=0.001 * |
| A/D treatment reported: | |||
| complementary, No. (%) | 2 (2.3) | 7 (4) | |
| psychotherapy, No. (%) | 5 (5.7) | 14 (7.9) | |
| ansioliticos and/or antidepressant, No. (%) | 11 (12.5) | 5 (2.8) | |
| drugs and psychotherapy, No. (%) | 5 (5.7) | 3 (1.7) | |
| Psychological treatment by telemedicine | 13 (14.8) | 12 (6.8) | |
| Psychological treatment suspended | 10 (11.3) | 2 (1.1) | |
| Psychological treatment in the past | 19 (21.6) | 55 (31.1) | |
| None (psychological treatment) | 44 (50) | 98 (55.4) | |
| GAD-7 score, mean, (SD) | 5.9 (4.8) | 5 (4.2) | p=0.167 ° |
| 0–4: minimal anxiety | 40 (46.5) | 92 (54.1) | |
| 5–9: mild anxiety | 30 (34.9) | 52 (30.6) | |
| 10–14: moderate anxiety | 8 (9.3) | 19 (11.2) | |
| 15–21: severe anxiety | 8 (9.3) | 7 (4.1) | |
| GAD-7 greater or equal to 10 No. (%) | 16 (18.60) | 26 (15.3) | |
| PHQ-9 score), mean, (SD) | 6.6 (5.2) | 6.2 (4.8) | p=0.752 ° |
| 0-4: No symptoms | 36 (43.4) | 74 (44.3) | |
| 5-9: Few symptoms | 25 (30.1) | 61 (36.5) | |
| 10-14: Moderate symptoms | 15 (18.1) | 21 (12.6) | |
| 15-19: Moderately/severe symptoms | 4 (4.8) | 7 (4.2) | |
| >20: Severe Depression | 3 (3.6) | 4 (2.4) |
Health Perception
The pwMS expressed concern for their MS course, considering themselves at higher risk and, in general, they were more worried for their health compared to controls (Figure 1) with a significative correlation with anxiety but not with depression. The concern for MS course and the perception to be at higher risk of infection were associated with A/D. Please refer to the Table 5A that reports this and all the correlations mentioned in the following paragraphs between A/D and the studied variables. On the other hand, controls didn’t consider themselves at higher risk but the concern for their health was also associated with A/D, with a closer correlation between their psychological status and the concern for their other chronic condition when present.
Figure 1.Significant differences between pwMS and controls in perception about “health” (box plot n. 1-3), in “media news” (box plot n. 4-6) and in “stay outside” (box plot n. 7) (p-values are according to exact Mann-Whitney U test).
All subjects were worried for their families, with a closer and significative correlation for controls compared to pwMS.
Job
PwMS with an employment contract appeared more anxious (p=0.0207) and depressed (p=0.0407) compared to controls and only the latter felt themselves protected from smart working (p=0.0120), that otherwise determined overwork (p=0.002).
Daily Coping Strategies
We observed in all subjects two adaptive strategies that improved the A/D psychological status: to stay focused on unusual activities and to keep busy on self-rewarding practical actions. Both should be remarked during psychological consultations, especially the latter which is more used (p=0.005) and more effective for pwMS (Figure 2).
On the other hand, the strategies that positively correlated with anxiety and depression in all the sample were: feeling stuck and doing anything; feeling the head elsewhere; feeling nervous; feeling hyperactive; eating to avoid thinking.
Moreover pwMS tended to adopt more than controls the following coping strategies, associated with psychological burden: thinking always about health issues, just listening to the news (Figure 2).
Figure 2.Significant differences between pwMS and controls in daily coping strategies (p-values are according to exact Mann-Whitney U test).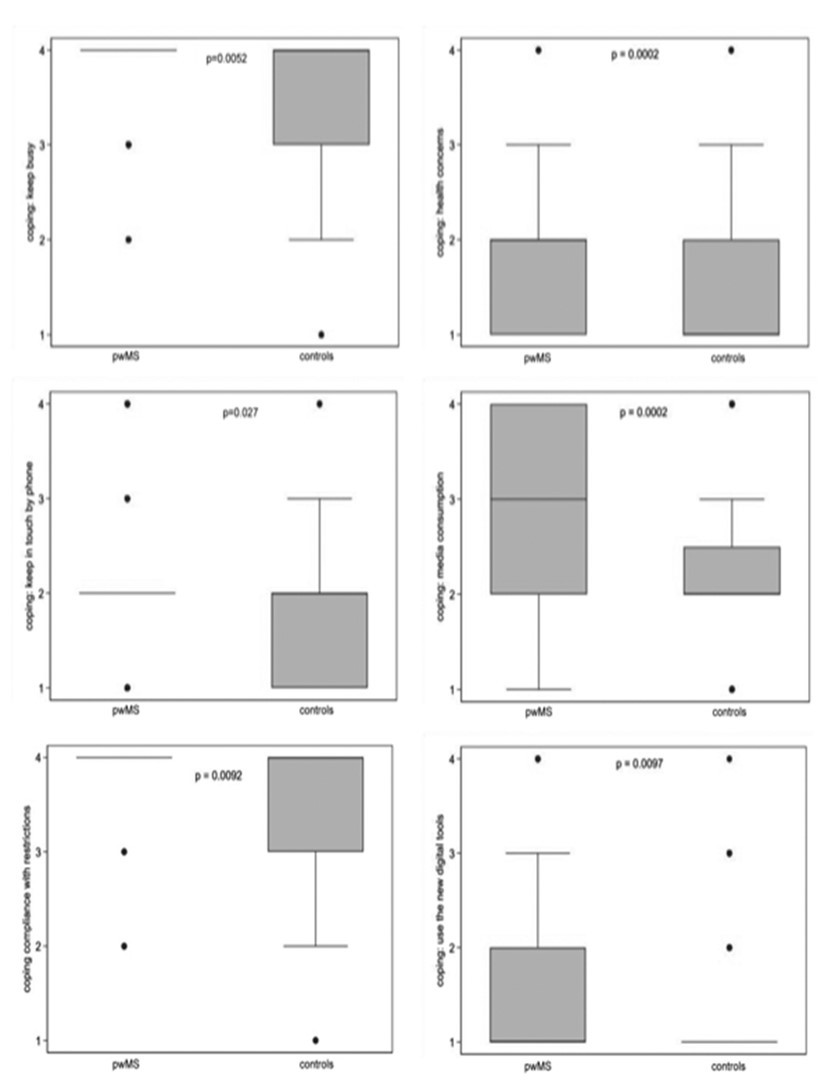
These themes should be investigated during the clinical interviews to provide psycho-educational support.
Empathy seemed to show a greater and significant emotional impact only in controls, as shown by these sentences: “I’m distressed for those who are sick and I can’t help”, “I'm always on the phone to make sure friends and family are safe”.
News
In general, the emotional reaction to media news was strictly associated with the psychological burden in all the subjects, and is expressed especially in these terms: feeling a weight on the stomach; sleeping badly; reflecting on the emergency; feeling hopeless, restless, pained. Compared to controls, pwMS reported more frequently to follow the news all day long, considering this more useful and reliable, in order to respect the restrictions and to feel protected (Figure 1). Psychological status didn’t correlate with these considerations in pwMS except for frequency of news listened; on the contrary, controls felt more anxious when they affirmed to doubt about the utility of the news and to reflect on that.
Family
In all subjects, psychological status was strongly associated with negative family relations. The burden increased the more the relatives were considered irritant, suffocating, unbearable.
Home
For pwMS the difficulty to stay at home was associated with living space (p=0.012) and not related to family as conversely happened in controls, who were only conditioned by stressful domestic relations.
Stay Outside
The discomfort of staying at home was similar in all subjects but pwMS reported more frequently the fear to go outside (Figure 1). Both factors correlated with anxiety and depression, even if the association was closer in controls, who seemed to tolerate worse the restrictions, possibly because they didn’t feel at higher risk to be infected.
Sport
PwMS practiced less physical activity compared to controls. Nearly 20% of subjects in both groups stopped the physical activity, but no difference in terms of A/D was detected compared to persons who continued sport. (PHQ-9: p=0.0984; GAD-7: p=0.1992).
SARS-CoV-2
We considered all the controls because no differences were observed in SARS-CoV-2 related variables selecting only the northern population. Among the subjects who reported the suspect to be infected by the virus, only the controls showed a significant psychological reaction. Participants reported a similar rate of persons deceased for SARS-CoV-2 among family, friend or neighbors and reacted with a comparable emotional response but in cases of mourning, controls were more frequently worried to be infected (p=0.026).
Discussion
The study received a good feedback by pwMS and the web survey represented a very useful tool, as other examples of telemedicine, in an outstanding period of restrictions 16. Despite the possible selection bias due to the voluntary enrollment, socio-demographic characteristics didn’t differ between groups and this was a favorable element which encouraged us to proceed with the comparison. Moreover, the geographical distribution of the sample didn’t determine a significant difference in the perception of SARS-CoV-2 related variables, as reported in other studies 17, 18, allowing us to consider the sample as a whole.
A/D rate in pwMS proved comparable with the results of other Italian surveys conducted during the SARS-CoV-2 lockdown even if collected with different questionnaires. Considering the clinical cut-off, Capuano 19 reported a similar rate of 16.4% for anxiety, evaluated with the State section of the State-Trait Anxiety Inventory, and a lower rate of 11.9% for depression, evaluated with the Beck Depression Inventory II (BDII>18).
Regarding the severity class of A/D symptoms, Zanghì 18 according to the Depression, Anxiety and Stress Scale, reported comparable data with a rate of 42.1% for mild/moderate anxiety class and a rate of 44.4% for mild/moderate depression class (Table 3).
Moreover we must consider that the results of psychological assessment might be influenced by the specific questionnaire administered and that we collected an emotional snapshot of the acute phase of the pandemic, without a follow up to check the evolution of the psychological reaction over time. For these reasons we decided to consider the PHQ-9 and GAD-7 normative data referred to pwMS and to the general population as additional control for each group.
Regarding the PHQ-9 tool, our findings (Table 3) are consistent with pwMS literature data collected before the pandemic; in fact Terrill 21 reported a mean score of 7.5 (5.5) point in 513 pwMS, and Amtmann 14 detected a mean score of 6.6 points in 455 pwMS with the following rate of depression for each frequency class: minimal = 42.4%; mild=33.2%; moderate=16.3%; severe=8.1%.
The PHQ-9 normative data in the general population shows a prevalence rate of moderate to high severity of depressive symptoms of 5.6% with a mean range of 2.9 (3.5) 22 while in our data controls reported three times higher scores.
Literature data concerning GAD-7 indicate a rate of 6.2% in the general population 23 with a mean score of 2.95 (3.3) 22 that are twice as much compared to our data in controls. Korostil 25 reported the rate of 19% in pwMS which is similar to our results.
In summary, A/D findings were similar to the published pre-pandemic data for pwMS and higher for the controls, considering pwMS and the normative data. These findings support the hypothesis that the psychological reaction of pwMS in the first period of lockdown was limited. In fact the A/D scores were not higher compared to the expected in pwMS. On the contrary the controls showed higher values than the normative ones, suggesting an acute psychological reaction. Maybe that PwMS mainly concentrated on the psychological reactions to the SARS-CoV-2 pandemic, dissociating the MS, also because the questions were not referred, as usual, only and specifically to the MS perception. Despite this possible limitation, the central role of MS in thoughts and emotions of pwMS is underlined by the answers about the health concern, by the coping strategies and by the importance of the correlation with A/D as described below and overall reported in Supplementary Table 2A. Furthermore we placed the A/D brief screening questionnaire at the end of the survey with the indication to consider the psychological state in general.
Looking at the variables studied, first of all health perception, pwMS considered themselves at higher risk for the infection, upon advice from experts and new regulatory norms, showing more caution and fear to go outside. So they might have been more resilient to tolerate the restrictions and the cohabiting relatives. When a suspect of infection occurred, PwMS tended to show lower A/D symptoms than controls.
The correlation between health themes and the psychological reaction resulted closer in controls, suggesting that the pandemic was the main trigger for them, while in pwMS other factors might be involved, first of all MS. Nevertheless pwMS with recent MS diagnosis, supposedly being more used to tolerate the change of daily habits, didn’t show more resilience in terms of lower A/D score. In a larger study 26 that share with us the relevant role of the personal coping to bear the lockdown, the time since diagnosis with other factors as gender, antidepressant, living arrangements or employment status didn't predict a impact of the pandemic on the personal life.
About daily life, most of the coping strategies were common in both groups. Staying active and focused on practical tasks resulted in the best adaptive strategy, being more effective in this fragile population, as reported in a similar Italian study and in the previously cited international survey 18, 26.
Despite this, pwMS selected more frequently some maladaptive strategies: they were more used to think about health, to continue by video calls the usual activities and to keep in contact by phone with relatives and friends, even if this increased anxiety (Figure 2). These daily habits should be inquired and supported during the clinical visits.
Media news showed an important and negative impact on A/D. PwMS reported to listen to the news more frequently compared to the controls but, even if they considered the news reliable and useful to keep on respecting the lockdown, these considerations didn’t affect their psychological status while the doubts on reliability of news increased anxiety in controls (Figure 1).
According with other studies the physical activity 27, the MS duration and employment status 26 were not associated with the psychological reaction during the lockdown. Job by itself is a vexed theme for pwMS 28 and represents a primary source of stress. Maybe for this reason the A/D scores were not associated with the actual changes in working habits, as happened for controls.
Conclusions
Despite the small sample and the possible selection bias due to the voluntary enrollment, these results might suggest that pwMS showed a proper psychological resilience during the first acute phase of the SARS-CoV-2 pandemic. They respected the restrictions more easily, being more aware of the priority of health. However, they tended more often to use phone and video calls and to focus on the media news and on health concerns, fueling A/D. Clinicians should pay attention to enquire about these specific maladaptive strategies considering the chance of a specific psychological intervention to support them in the different phases of the pandemic.
Ethical Compliance Section
Funding
The authors have no funding to disclose.
Compliance with Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Milano Area 3 Ethic Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Digital Informed consent was obtained from all individual adult participants included in the study.
Acknowledgement
To all the people who actively and voluntarily participated in the study in such a difficult and chaotic period of life.
Appendix
| Section | Content |
| Title | “DIMMI COME STAI” “How are you” survey |
| I | Includes the study and the privacy disclosures with the informed consent. |
| II | Contains multiple choice questions about: socio-demographics, MS anamnestic data and current treatment, previous history of anxiety and depression with related treatment. |
| a. Socio-demographics | |
| 1. Phantasy code: xxx | |
| 2. Gender: male/female | |
| 3. Age: aa | |
| 4. Province of residence (or actual domicile if differente): xxx | |
| b. Multiple sclerosis/chronic disease anamnestic data and current treatment | |
| 5. The onset date multiple sclerosis/chronic disease was: dd/mm/yyyy | |
| *5bis. My health status is: low/enough/discrete/good | |
| 6. I am being treated for multiple sclerosis/chronic disease: Yes/no/Not yet (I'm completing the clinical investigations) | |
| *6bis. If you want, indicate the name of the disease you are being treated for: xxxxxx | |
| 7. I am being treated for multiple sclerosis/chronic disease with the following drug: xxxx | |
| 8. During this SARS-CoV-2 emergency period, I am continuing the therapy: as scheduled/it is suspended/it has been postponed/it is given to me in a hospital closer to my residence | |
| c. Previous history of anxiety and depression with related treatment | |
| 9. I suffer from anxious depressive symptoms: no/no, I have suffered from this in the past/yes, I'm currently suffering | |
| 10. I am being treated with: anxiolytics-antidepressants/anxiolytics-antidepressants and psychotherapy/psychotherapy/natural therapies/I don’t follow (or have not followed) any treatment | |
| 11. I am continuing the psychological treatment: I've ended the psychological treatment in the past/I suspended the psychological treatment/I’m continuing the psychological treatment by phone | |
| d. Satisfaction with the information received by the MS Center | |
| 12. I succeeded successfully to communicate with my referral medical centre/specialist for information and practical guidance: I got no answer-I got effective answers (1-10) | |
| III | Refers to the health perception, the need for economic or logistic support and the lifestyle habits during the SARS-CoV-2 restrictions |
| a. health concern | |
| 13. How did you react at the beginning of the SARS-CoV-2 emergency? | |
| 13a. I worried about myself: not at all/quite/much/very very much (0-3) | |
| 13b. I worried about my family: not at all/quite/much/very very much (0-3) | |
| 13c. I felt more at risk than other people: not at all/quite/much/very very much (0-3) | |
| 13d. I worried about my illness: not at all/quite/much/very very much (0-3) | |
| b. need for economic or logistic support | |
| 14. Have you asked for support from the associations or the public institutions?: I didn't ask for support/I have not received support despite the request/I received support for food or other types of activities | |
| c. everyday life coping strategies | |
| 15. How are you acting with respect to the SARS-CoV-2 emergency ? (Please ask for each sentences: never/some days/for more than half of the days/almost every day) (1-4) | |
| 15a. I respect the restrictions, they make me feel safe | |
| 15b. Restrictions make me nervous | |
| 15c. I just listen to the information | |
| 15d. I feel stuck and can't do anything | |
| 15e. I'm hyperactive | |
| 15f. I keep busy: practical actions gratify me | |
| 15g. I use the time to do things I usually wouldn't do and I can stay focused | |
| 15h. My head’s always elsewhere, I can’t concentrate | |
| 15i. I always think about health issues | |
| 15l. I pray and trust in God | |
| 15m. I try to anticipate what will happen | |
| 15n. I'm always on the phone to make sure friends and family are okay | |
| 15o. I arranged to continue my activities by video call | |
| 15p. I refuse to use video calls or distract myself, it is not a time to think about futile things | |
| 15q. They are exaggerating the problem | |
| 15r. I try not to think about it by eating | |
| 15s. I’m distressed for those who are sick and I can’t help | |
| 15t. I try to defuse the situation with my loved ones | |
| d. home and the family relationship | |
| 16. How many people live with you, in the same house? (indicates the number of adults and minors): nn | |
| 17. Is there enough space for everyone?: not at all-a lot (1-4) | |
| 18. Right now, how often the friends and relatives you interact with more frequently, appear: | |
| 18a. missing: never/some days/for more than half of the days/almost every day | |
| 18b. irritant: never/some days/for more than half of the days/almost every day | |
| 18c. enjoy the company: never/some days/for more than half of the days/almost every day | |
| 18d. suffocating: never/some days/for more than half of the days/almost every day | |
| 18e. stimulating: never/some days/for more than half of the days/almost every day | |
| 18f. unbearable: never/some days/for more than half of the days/almost every day | |
| 19. Can you stay indoors: easily-it causes me enormous discomfort (1-4) | |
| 20. When you go out, you feel: terrified-happy (1-4) | |
| e. physical activities | |
| 21. Please select all applicable items about physical exercise and/or physiotherapy: | |
| 21a. I can't do it for physical reasons: true/false | |
| 21b. I wouldn't do it anyway, I don't like it: true/false | |
| 21c. I am not in treatment: true/false | |
| 21d. It is usually tiring, so I’m taking the opportunity to rest: true/false | |
| 21e. I feel the need but it has been interrupted: true/false | |
| 21f. I feel the need and continue it at home, as I can: true/false | |
| f. job changes | |
| 22. What is your current employment status? (please select all applicable items) | |
| 22a. I am working as usual: true/false | |
| 22b. I work according to different schedules and methods as per company indications: true/false | |
| 22c. I’m working from home: true/false | |
| 22d. I'm on vacation / layoffs: true/false | |
| 22e. I am self-employed and cannot work due to restrictions: true/false | |
| 22f. I don't have a job: true/false | |
| 22g. I am a homemaker: true/false | |
| 23. Since the beginning of the SARS-CoV-2 restrictions, which of the following work-related statements do you agree with? (please select all the applicable items) | |
| 23a. I am working too much: true/false | |
| 23b. I am a housewife and housekeeping is more demanding: true/false | |
| 23c. Luckily I am working, so I keep busy: true/false | |
| 23d. I am missing work: true/false | |
| 23e. I am missing the work environment: true/false | |
| 23f. I am relieved not to have to leave for work: true/false | |
| 23g. I don't work and I feel better because I am less fatigued: true/false | |
| 23h. I am a housewife and now my relatives are helping me: true/false | |
| 23i. I am worried about losing my job: true/false | |
| 23l. I am worried about the economic aspect: true/false | |
| g. impact of media news | |
| 24. Are you listening to the radio and television information on the SARS-CoV-2 emergency?: I follow the news and updates as much as possible/many times a day/daily/I try to avoid them | |
| 25.How do you consider the media news? | |
| 25a. News are useful: not at all/quite/much/very very much | |
| 25b.After news I feel a weight on my stomach: not at all/quite/much/very very much | |
| 25c. If I listen to news in the evening I happen to sleep badly: not at all/quite/much/very very much | |
| 25d. News are not always reliable: not at all/quite/much/very very much | |
| 25e. News make me pained: not at all/quite/much/very very much | |
| 25f. After news, I don't think that the emergency: not at all/quite/much/very very much | |
| 25g. News make me lose hope: not at all/quite/much/very very much | |
| 25h. News agitate me: not at all/quite/much/very very much | |
| 25i. News motivate me to follow the restrictions: not at all/quite/much/very very much | |
| 25l. News make me think: not at all/quite/much/very very much | |
| IV | Contain the feared or objective SARS-CoV-2 symptoms, the mourning of relatives, friends or neighbors caused by the virus. |
| a. feared or objective SARS-CoV-2 symptoms | |
| 26. Are you in quarantine due to the SARS-CoV-2 virus?: yes/noyes, together with other family members | |
| 27. Have you had symptoms caused by the SARS-CoV-2 virus? | |
| yes/no/I’m/was afraid of having any/I had the suspicion but it was not confirmed by the doctors | |
| b. mourning of relatives, friends or neighbors caused by the virus. | |
| 28. Are you in mourning for the death of persons close to you due to SARS-CoV-2 virus? (please select all applicable items): yes, family members/yes, friends/yes, acquaintances/yes, people who live near me/no, none | |
| V | Consist of the two following brief self administered questionnaires about the psychological status and of the final considerations and tips |
| 29.The Patient Health Questionnaire (PHQ-9) | |
| 30. The 7-items Generalized Anxiety Disorder Scale (GAD-7) | |
| 31. Final considerations (if you wish, write here in detail): xxx | |
| 32. Tips (if you wish, write here what you would add or change in the questionnaire): xxx |
Table 5A. Comparisons of lifestyle, habits and contextual variables between groups by the exact Mann-Whitney U test and correlations with PHQ-9 and GAD-7 psychological score using the Spearman's ρ
| PHQ-9 | GAD-7 | ||||||||||||||
| pwMS | controls | pwMS | controls | ||||||||||||
| Spearman's correlation test | Mann Whitney test | ||||||||||||||
| Contextual variables | n. obs | rho | p | n. obs | rho | p | n. obs | rho | p | n. obs | rho | p | N. MS | controls | P |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Concern for health | 79 | 0.126 | 0.268 | 155 | 0.223 | 0.005 | 79 | 0.246 | 0.029 | 155 | 0.184 | 0.022 | 84 | 171 | 0.0003 |
| of relatives | 79 | 0.173 | 0.128 | 155 | 0.257 | 0.001 | 79 | 0.283 | 0.011 | 155 | 0.208 | 0.009 | 85 | 173 | 0.687 |
| to be at higher risk | 79 | 0.236 | 0.037 | 155 | 0.048 | 0.549 | 79 | 0.228 | 0.044 | 155 | 0.119 | 0.166 | 85 | 168 | 0.00001 |
| for chronic condition/MS | 79 | 0.341 | 0.002 | 155 | 0.306 | 0.0001 | 79 | 0.350 | 0.002 | 155 | 0.339 | 0.00001 | 84 | 160 | 0.00001 |
| Coping | |||||||||||||||
| I keep busy | 71 | -0.581 | 0.00001 | 161 | -0.236 | 0.003 | 72 | -0.440 | 0.0001 | 160 | -0.139 | 0.079 | 87 | 173 | 0.005 |
| I concentrate on unusual things | 71 | -0.331 | 0.005 | 161 | -0.263 | 0.001 | 72 | -0.292 | 0.0129 | 160 | -0.231 | 0.0033 | 85 | 174 | 0.466 |
| I try to defuse the situation with my loved ones | 71 | -0.142 | 0.239 | 161 | -0.058 | 0.466 | 72 | -0.181 | 0.128 | 160 | -0.007 | 0.927 | 86 | 168 | 0.134 |
| They are exaggerating the problem | 71 | -0.003 | 0.982 | 161 | -0.015 | 0.850 | 72 | -0.066 | 0.581 | 160 | -0.099 | 0.212 | 83 | 168 | 0.417 |
| Restrictions make me nervous | 71 | 0.420 | 0.0003 | 161 | 0.263 | 0.001 | 72 | 0.524 | 0.00001 | 160 | 0.257 | 0.001 | 85 | 172 | 0.424 |
| I feel stuck and can't do anything | 71 | 0.492 | 0.00001 | 161 | 0.493 | 0.00001 | 72 | 0.498 | 0.00001 | 160 | 0.454 | 0.00001 | 83 | 171 | 0.176 |
| I can’t concentrate | 71 | 0.621 | 0.00001 | 161 | 0.676 | 0.00001 | 72 | 0.656 | 0.00001 | 160 | 0.656 | 0.00001 | 85 | 172 | 0.751 |
| I refuse to use video calls or distract myself, it is not this the time | 71 | 0.141 | 0.239 | 161 | 0.067 | 0.399 | 72 | 0.214 | 0.071 | 160 | 0.055 | 0.492 | 81 | 169 | 0.067 |
| I pray and trust in God | 71 | 0.163 | 0.174 | 161 | 0.122 | 0.124 | 72 | 0.123 | 0.302 | 160 | 0.153 | 0.053 | 84 | 171 | 0.289 |
| I'm hyperactive | 71 | 0.186 | 0.119 | 161 | 0.322 | 0.00001 | 72 | 0.338 | 0.004 | 160 | 0.423 | 0.00001 | 84 | 173 | 0.378 |
| I don’t think by eating | 71 | 0.457 | 0.0001 | 161 | 0.402 | 0.00001 | 72 | 0.348 | 0.003 | 160 | 0.352 | 0.00001 | 82 | 168 | 0.247 |
| I try to anticipate what will happen | 71 | 0.213 | 0.075 | 161 | 0.150 | 0.057 | 72 | 0.292 | 0.013 | 160 | 0.186 | 0.0187 | 84 | 170 | 0.403 |
| I’m worried because of people being ill | 71 | -0.011 | 0.925 | 161 | 0.360 | 0.00001 | 72 | 0.173 | 0.147 | 160 | 0.412 | 0.00001 | 85 | 169 | 0.642 |
| I arranged to continue my activities by video call | 71 | -0.084 | 0.484 | 161 | -0.043 | 0.587 | 72 | -0.087 | 0.469 | 160 | 0.022 | 0.783 | 84 | 173 | 0.01 |
| I respect the restrictions, they make me feel safe | 71 | -0.037 | 0.756 | 161 | -0.051 | 0.522 | 72 | -0.032 | 0.791 | 160 | -0.046 | 0.567 | 86 | 175 | 0.009 |
| I always think about health issues | 71 | 0.296 | 0.012 | 161 | 0.352 | 0.00001 | 72 | 0.457 | 0.0001 | 160 | 0.360 | 0.00001 | 85 | 170 | 0.0002 |
| I just listen to the information | 71 | 0.291 | 0.014 | 161 | 0.254 | 0.001 | 72 | 0.281 | 0.017 | 160 | 0.162 | 0.041 | 85 | 172 | 0.0002 |
| I'm always on the phone to make sure my beloved are okay | 71 | 0.139 | 0.247 | 161 | 0.297 | 0.0001 | 72 | 0.292 | 0.013 | 160 | 0.334 | 0.00001 | 85 | 171 | 0.027 |
| Beloved perception | |||||||||||||||
| irritant | 78 | 0.390 | 0.0004 | 156 | 0.403 | 0.00001 | 82 | 0.375 | 0.0005 | 156 | 0.435 | 0.00001 | 85 | 165 | 0.838 |
| missing | 78 | 0.023 | 0.844 | 156 | 0.360 | 0.00001 | 82 | 0.077 | 0.494 | 156 | 0.293 | 0.0002 | 86 | 173 | 0.253 |
| suffocating | 78 | 0.451 | 0.00001 | 156 | 0.350 | 0.00001 | 82 | 0.420 | 0.0001 | 156 | 0.377 | 0.00001 | 86 | 164 | 0.802 |
| stimulating | 78 | -0.029 | 0.802 | 156 | -0.098 | 0.221 | 82 | -0.030 | 0.786 | 156 | -0.117 | 0.147 | 85 | 165 | 0.203 |
| unbearable | 78 | 0.288 | 0.011 | 156 | 0.350 | 0.00001 | 82 | 0.360 | 0.001 | 156 | 0.356 | 0.00001 | 85 | 163 | 0.673 |
| enjoy the company | 78 | 0.159 | 0.165 | 156 | 0.014 | 0.858 | 82 | 0.184 | 0.097 | 156 | -0.054 | 0.501 | 85 | 163 | 0.694 |
| living space | -> | -> | -> | -> | -> | -> | -> | -> | -> | -> | -> | -> | 87 | 170 | 0.121 |
| happy to go out | 80 | -0.265 | 0.018 | 167 | -0.263 | 0.001 | 84 | -0.245 | 0.025 | 167 | -0.329 | 0.00001 | 85 | 177 | 0.029 |
| discomfort to stay at home | 80 | 0.256 | 0.022 | 167 | 0.227 | 0.003 | 84 | 0.356 | 0.001 | 167 | 0.156 | 0.043 | 88 | 176 | 0.700 |
| Media news reaction | |||||||||||||||
| The frequency of listening news | -> | -> | -> | -> | -> | -> | 87 | 0.047 | 0.664 | 166 | 0.039 | 0.614 | 88 | 176 | 0.058 |
| News are useful | 82 | -0.184 | 0.098 | 86 | -0.152 | 0.163 | 165 | 0.177 | 0.023 | 87 | 172 | 0.0003 | |||
| I feel a weight on my stomach | 79 | 0.452 | 0.00001 | 83 | 0.494 | 0.00001 | 162 | 0.590 | 0.00001 | 83 | 164 | 0.962 | |||
| I sleep badly | 81 | 0.513 | 0.00001 | 84 | 0.490 | 0.00001 | 162 | 0.469 | 0.00001 | 84 | 165 | 0.655 | |||
| Are not always reliable | 82 | 0.096 | 0.389 | 85 | 0.033 | 0.765 | 163 | 0.052 | 0.511 | 85 | 167 | 0.017 | |||
| Make me pained | 82 | 0.183 | 0.100 | 86 | 0.156 | 0.150 | 161 | 0.390 | 0.00001 | 86 | 166 | 0.866 | |||
| I always think about the emergency | 82 | 0.3749 | 0.0005 | 85 | 0.548 | 0.00001 | 160 | 0.395 | 0.00001 | 85 | 163 | 0.398 | |||
| Make me hopeless | 82 | 0.5598 | 0.00001 | 85 | 0.607 | 0.00001 | 161 | 0.435 | 0.00001 | 85 | 164 | 0.892 | |||
| I fell agitate | 82 | 0.5619 | 0.00001 | 86 | 0.611 | 0.00001 | 163 | 0.541 | 0,00001 | 86 | 166 | 0,513 | |||
| Motivate me to respect the restrictions | 83 | -0.1201 | 0,276 | 86 | 0,002 | 0,987 | 162 | 0.061 | 0,439 | 66 | 166 | 0,002 | |||
| Make me thoughtful | 82 | -0.0762 | 0,496 | 86 | -0,023 | 0,831 | 167 | 0.178 | 0,022 | 86 | 173 | 0,751 | |||
| PHQ_tot | 79 | 1 | - | 155 | 1 | - | 79 | 0,781 | 0.00001 | 155 | 0.792 | 0,00001 | 83 | 167 | 0,752 |
| GAD_tot | 79 | 0.7809 | 0,00001 | 155 | 0,792 | 0,00001 | 79 | 1 | - | 155 | 1 | - | 87 | 167 | 0,167 |
| EDSS | 83 | 0,1284 | 0,247 | -> | -> | -> | 83 | -0,672 | 0,546 | -> | -> | -> | -> | -> | -> |
References
- 1.Howard J, Trevick S, D S Younger. (1996) . , Epidemiology of Multiple Sclerosis. Neurol Clin 34(4), 919-939.
- 2.R A Marrie, Reingold S, Cohen J. (2015) The incidence and prevalence of psychiatric disorders in multiple sclero-sis: a systematic review. , Mult Scler 21(3), 305-17.
- 3.D C Mohr, Cox D. (2001) Multiple Sclerosis: Empirical Literature for the Clinical Health Psychologist. , Journal of Clinical Psychology 57(4), 479-499.
- 4.Ornell F, J B Schuch, A O Sordi. (2020) Pandemic fear’’ and COVID-19: mental health burden and strategies. , Braz J Psychiatry 42(3), 232-235.
- 5.Wu C, Chen X, Cai Y. (2020) . Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan , China, JAMA Intern Med 180(7), 934-943.
- 6.Pfefferbaum B, C S North. (2020) . , Mental Health and the Covid-19 Pandemic N Engl J Med 383, 510-512.
- 7.A J Thompson, B L, Barkhof F. (2018) Diagnosis of multiple sclerosis:. , Lancet Neurol 17, 162-173.
- 8.R L Spitzer, Kroenke K, Williams J B W. (2006) A Brief Measure for Assessing Generalized Anxiety Disorder. The GAD-7. Arch Intern Med, 166 : 1092-1097.
- 9.Kroenke K, R L Spitzer, J B Williams. (2001) The PHQ-9: validity of a brief depression severity measure. , J Gen Intern Med 16(9), 606-13.
- 10.American Psychiatric Association (2000) . Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (Text Revision), 4th ed , Washington, DC: .
- 11.Lowe B, Decker O, Muller S. (2008) Validation and standardization of the Generalized Anxiety Disorder Screen-er (GAD-7) in the general population. , Med Care 46, 266-274.
- 12.Honarmand K, Feinstein A. (2009) Validation of the Hospital Anxiety and Depression Scale for use with multiple scle-rosis patients. , Mult Scler 15, 1518-1524.
- 13.Patrick S, Connick P. (2019) Psychometric properties of the PHQ-9 depression scale in people with multiple sclerosis: A systematic review. 14(2), 0197943.
- 14.Amtmann D. (2014) . Comparing CESD-10, PHQ-9, and PROMIS Depression Instruments in Individuals with Mul-tiple Sclerosis. Rehabil Psychol 59(2), 220-229.
- 15.J F Kurtzke. (1983) Rating neurological impairment in multiple sclerosis: an expanded disability status scale (EDSS). , Neurology 33, 1444-1452.
- 16.Capra R, Mattioni F. (2020) Tele-health in neurology: an indispensable tool in the management of the SARS‐CoV‐2 epidemic. , Journal of Neurology 267, 1885-1886.
- 17.Forte G, Favieri F, Tambelli R, Casagrande M. (2020) The enemy which sealed the world: effects of COVID-19 diffu-sion on the psychological state of the Italian population. , J Clin Med 9(6), 1802.
- 18.Donisi V, Gajofatto A, M A, Gobbin F, I M Busch et al. (2021) Insights for Fostering Resilience in Young Adults With Multiple Sclerosis in the Aftermath of the COVID-19 Emergency: An Italian Survey. , Front. Psychiatry 11, 588275.
- 19.Capuano R, Altieri M, Bisecco A. (2021) Psychological consequences of COVID-19 pandemic in Italian MS pa-tients: signs of resilience?. , J Neurol 268, 743-750.
- 20.Zanghì A. (2020) Mental health status of relapsing-remitting multiple sclerosis Italian patients returning to work soon after the easing of lockdown during COVID-19 pandemic: A monocentric experience. , Mult Scler Relat Disord 46, 102561.
- 21.A L Terrill, Hartoonian N, Beier M. (2015) The 7-item Generalized Anxiety Disorder Scale as a tool for measuring generalized anxiety in multiple sclerosis. , Int J MS Care 17(2), 49-56.
- 22.R D Kocalevent, Hinz A, Brähler E. (2013) Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. , Gen Hosp Psychiatry 35(5), 551-5.
- 23.Kroenke K, R L Spitzer, J B Williams. (2007) Anxiety disorders in primary care: prevalence, impairment, comor-bidity, and detection. , Ann Intern Med 146, 317-325.
- 24.Löwe B, Decker O, Müller S. (2008) Validation and standardization of the Generalized Anxiety Disorder Screen-er (GAD-7) in the general population. , Med Care 46(3), 266-74.
- 25.Korostil M, Feinstein A. (2007) Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 13, 67-72.
- 26.Morris-Bankole H, A K Ho. (2021) The COVID-19 Pandemic Experience in Multiple Sclerosis: The Good, the Bad and the Neutral. , Neurol Ther 10, 279-291.
